Final ID: TAC282
Combination Therapy with ACEIs/ARBs and β-Blockers Reduces Basal Inflammation in Heart Failure Patients: A Cross-Sectional Observational Study
Abstract Body: Introduction
Inflammation is increasingly recognized as a contributor to heart failure progression, and elevated basal inflammation can begin as early as stage A of the disease. While neurohormonal blockades with angiotensin-converting enzyme inhibitors (ACEIs), angiotensin receptor blockers (ARBs), and β-blockers are standard for heart failure treatment, their specific effects on inflammatory biomarkers remain unclear.
Hypothesis
We hypothesized that combination therapy with ACEIs/ARBs and β-blockers reduces basal inflammatory cytokine levels more effectively than monotherapy in heart failure patients.
Methods
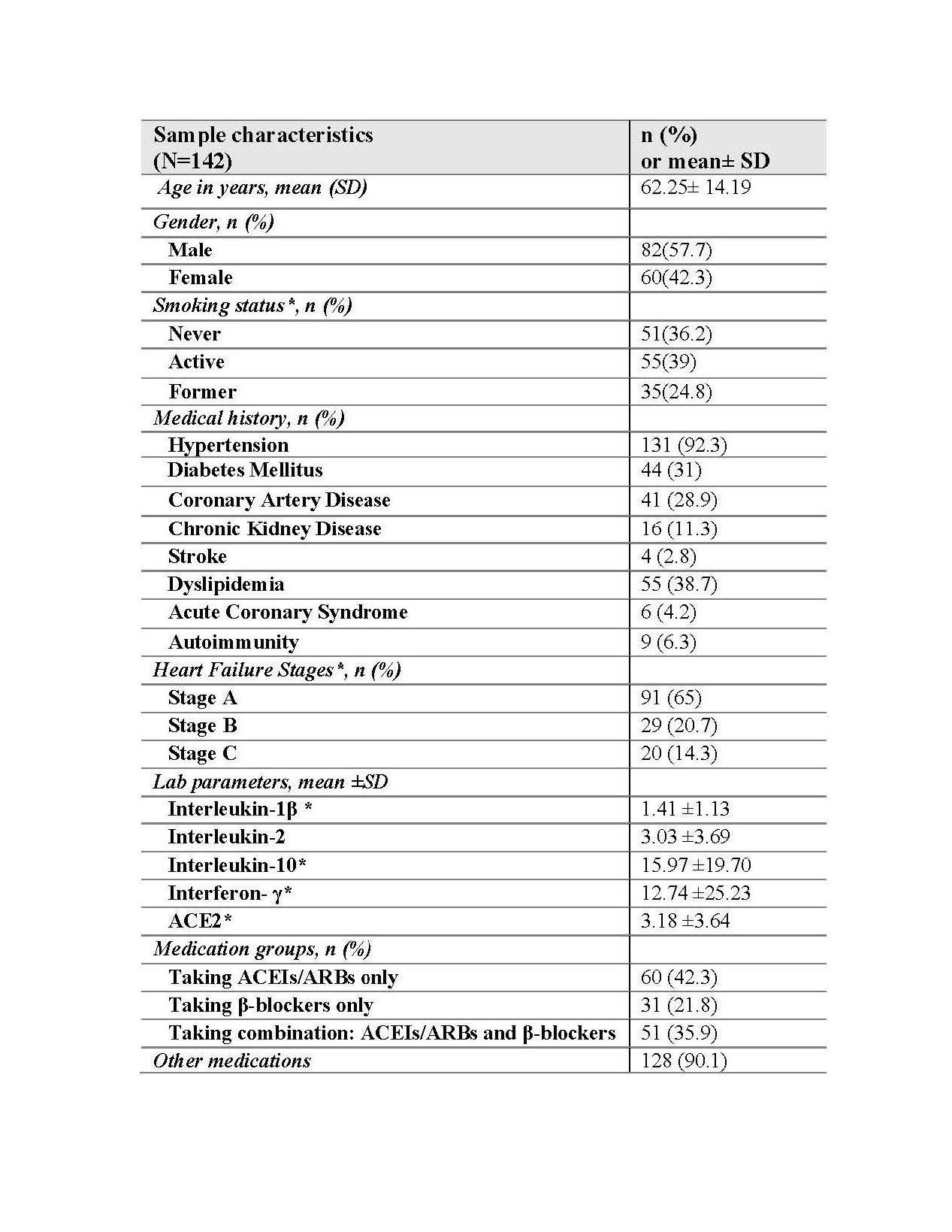
Following ACC/AHA guidelines, we conducted a cross-sectional observational study combining retrospective chart review and prospective blood collection at the American University of Beirut Medical Center. A total of 142 patients (mean age: 62.3 ± 14.2 years; 57.7% male) with stage A to C heart failure, were included. Patients were grouped by treatment: ACEIs/ARBs alone (42.3%), β-blockers alone (21.8%), or combination therapy of both (35.9%). Plasma levels of IL-1β, IL-2, IL-10, IFN-γ, and ACE2 were quantified using enzyme-linked immunosorbent assays (ELISA). Linear regression models adjusted for age, sex, heart failure stage, smoking status, and number of comorbidities, were implemented.
Results
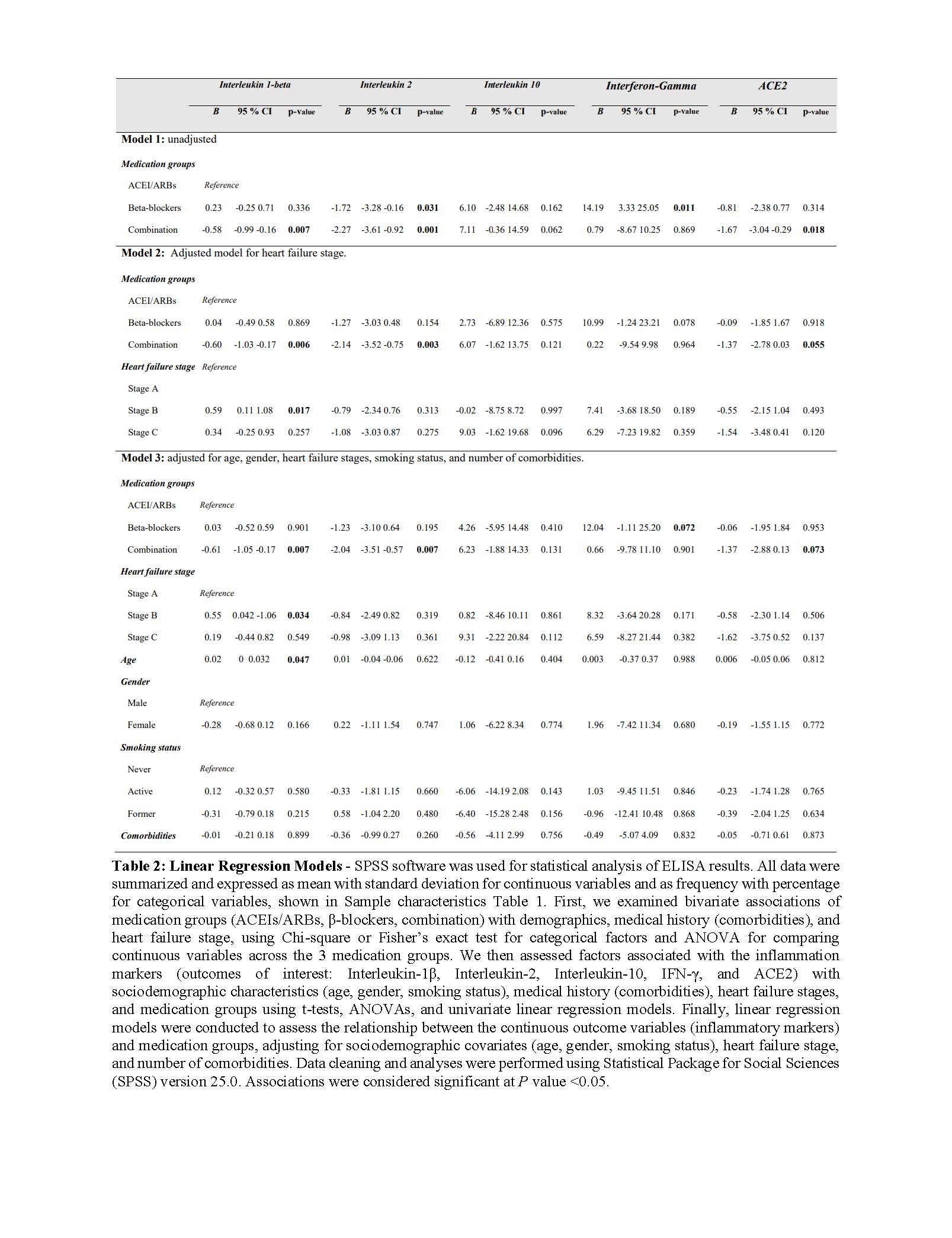
Patients on combination therapy had significantly lower IL-1β (B = -0.61, p = 0.007) and IL-2 (B = -2.04, p = 0.007) levels compared to those on ACEIs/ARBs alone. β-blocker monotherapy was associated with significantly elevated IFN-γ (B = 14.19, p = 0.011) that was not observed with dual treatment. ACE2 levels were significantly lower in the combination group (B = -1.67, p = 0.018) in unadjusted analysis, but this association was attenuated after adjustment (p = 0.07). IL-10 levels did not differ significantly between groups.
Conclusion
Combination therapy with ACEIs/ARBs and β-blockers appears to more effectively suppress pro-inflammatory cytokines than monotherapy, independent of ACE2 expression. These findings highlight a potential anti-inflammatory advantage of dual therapy in heart failure. Limitations include modest sample size and overrepresentation of stage A patients, which may affect generalizability. Additional analyses of TNF-α, IL-6, and CRP are ongoing to strengthen our findings. Future studies will include RNA sequencing on isolated peripheral blood mononuclear cells (PBMCS) to further elucidate the immuno-modulatory mechanisms behind these findings.
Inflammation is increasingly recognized as a contributor to heart failure progression, and elevated basal inflammation can begin as early as stage A of the disease. While neurohormonal blockades with angiotensin-converting enzyme inhibitors (ACEIs), angiotensin receptor blockers (ARBs), and β-blockers are standard for heart failure treatment, their specific effects on inflammatory biomarkers remain unclear.
Hypothesis
We hypothesized that combination therapy with ACEIs/ARBs and β-blockers reduces basal inflammatory cytokine levels more effectively than monotherapy in heart failure patients.
Methods
Following ACC/AHA guidelines, we conducted a cross-sectional observational study combining retrospective chart review and prospective blood collection at the American University of Beirut Medical Center. A total of 142 patients (mean age: 62.3 ± 14.2 years; 57.7% male) with stage A to C heart failure, were included. Patients were grouped by treatment: ACEIs/ARBs alone (42.3%), β-blockers alone (21.8%), or combination therapy of both (35.9%). Plasma levels of IL-1β, IL-2, IL-10, IFN-γ, and ACE2 were quantified using enzyme-linked immunosorbent assays (ELISA). Linear regression models adjusted for age, sex, heart failure stage, smoking status, and number of comorbidities, were implemented.
Results
Patients on combination therapy had significantly lower IL-1β (B = -0.61, p = 0.007) and IL-2 (B = -2.04, p = 0.007) levels compared to those on ACEIs/ARBs alone. β-blocker monotherapy was associated with significantly elevated IFN-γ (B = 14.19, p = 0.011) that was not observed with dual treatment. ACE2 levels were significantly lower in the combination group (B = -1.67, p = 0.018) in unadjusted analysis, but this association was attenuated after adjustment (p = 0.07). IL-10 levels did not differ significantly between groups.
Conclusion
Combination therapy with ACEIs/ARBs and β-blockers appears to more effectively suppress pro-inflammatory cytokines than monotherapy, independent of ACE2 expression. These findings highlight a potential anti-inflammatory advantage of dual therapy in heart failure. Limitations include modest sample size and overrepresentation of stage A patients, which may affect generalizability. Additional analyses of TNF-α, IL-6, and CRP are ongoing to strengthen our findings. Future studies will include RNA sequencing on isolated peripheral blood mononuclear cells (PBMCS) to further elucidate the immuno-modulatory mechanisms behind these findings.
More abstracts on this topic:
Additive Value of Lipoprotein(a), Remnant Cholesterol, and Inflammation for Risk Stratification of Myocardial Infarction: Evidence from the UK Biobank
Kazibwe Richard, Schaich Christopher, Kingsley Jeffrey, Rikhi Rishi, Namutebi Juliana, Chevli Parag, Mirzai Saeid, Shapiro Michael
Beta blockers and calcium channel blockers in pre-symptomatic patients with hypertrophic cardiomyopathy: prevalence, discontinuation, and effectivenessBradlow William, Sehnert Amy, Bastien Arnaud, Blizard Perry, Ripoll-vera Tomas, Pericas Pau, Fudim Marat, Balu Suresh, Hintze Bradley, Salah Husam, Patel Manesh, Elgui Kevin, Foucher Aurelie, Charron Philippe, Klopfenstein Quentin, Balazard Felix, Trichelair Paul, Touzot Maxime, Micsinai Balan Mariann, Van Haelst Paul, Sandler Belinda