Final ID: TAC106
Pharmacokinetic Interactions Between Beta Blockers and CYP2D6 Inhibiting Antidepressants (Selective Serotonin Reuptake Inhibitors, Duloxetine and Bupropion) : A Systematic Review and Meta Analysis
Abstract Body: Introduction: Antihypertensive and psychotropic medications in same patient creates issues. Beta-blockers when co-administered with SSRIs/SNRIs, enzymes in the body, known as CYP450, can produce additional pharmacological effects that may influence outcomes and side effects. Interactions between beta-blockers and antidepressants calculates to identify areas where safety and success of treatment could be improved.
Hypothesis: Depression and hypertension patients treated with the selected CYP2D6-dependent beta-blockers with common antidepressants showed 15-20% greater decrease in systolic blood pressure and increased (by 25%) chance of developing bradycardia.
Methods: PRISMA guidelines was followed. PubMed, Embase, and Cochrane Library was searched upto May 2025. Eligible studies evaluated pharmacokinetic interactions between β-blockers and CYP2D6-inhibiting SSRIs, duloxetine, or bupropion in adults aged >20 years. Data on drug plasma concentrations, clearance, area under the curve (AUC) were extracted. Statistical analyses conducted using RevMan 5.4, with pooled effect estimates calculated via random-effects models. Heterogeneity assessed using I2 statistics to quantify degree of variability.
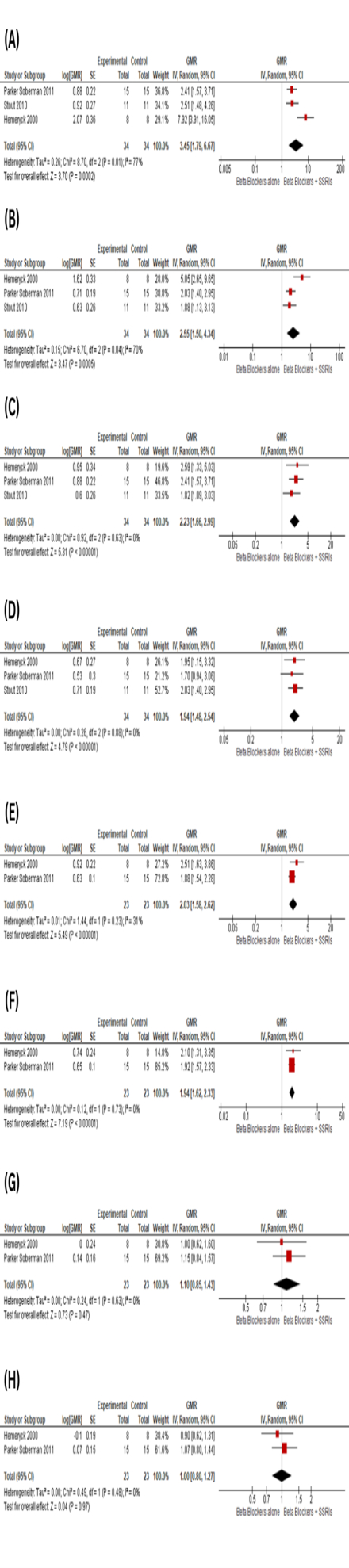
Results: Meta-analysis of 65 participants demonstrated pharmacokinetic interactions between beta-blockers and antidepressant medications. S-enantiomers of beta-blockers with SSRIs, AUC increased by 2.55 (95% CI: 1.50–4.34), Cmax by 1.94 (95% CI: 1.48–2.54), half-life by 1.94 (95% CI: 1.62–2.33), with no Tmax change. Heterogeneity was moderate- high for AUC (I2 = 70–77%) and low for Cmax/half-life (I2 = 0%).
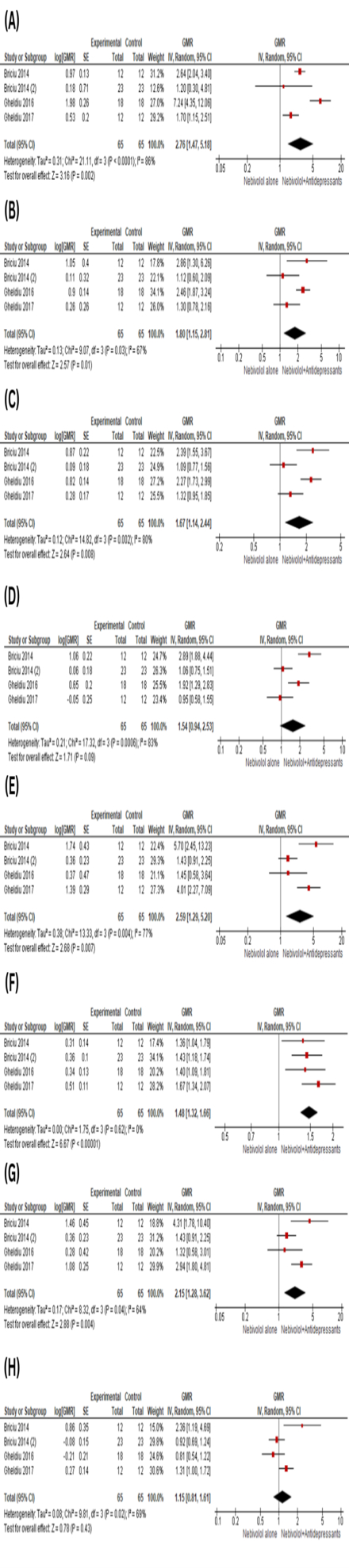
Nebivolol with antidepressants, AUC increased by 2.76 (95% CI: 1.47–5.18), Cmax by 1.67 (95% CI: 1.14–2.44), half-life by 1.80 (95% CI: 1.15–2.81). OH-Nebivolol metabolite exhibited greater effects: AUC by 2.59 (95% CI: 1.29–5.20), Cmax by 1.48 (95% CI: 1.32–1.66), half-life by 2.15 (95% CI: 1.28–3.62). Tmax showed no differences. Analysis revealed heterogeneity moderate- high (I2 = 64–86%), except Cmax of metabolite (I2 = 0%).
Conclusion: CYP2D6-metabolized beta-blockers (e.g., metoprolol, carvedilol) are altered by concomitant SSRI/ antidepressant use, increasing systemic exposure, higher plasma levels, and prolonged half-life, potentially intensifying therapeutic and adverse effects. In contrast, beta-blockers (atenolol and nadolol), remain unaffected. Clinicians should assess drug interactions, dose adjustments, and implement monitoring to ensure optimal outcomes.
Hypothesis: Depression and hypertension patients treated with the selected CYP2D6-dependent beta-blockers with common antidepressants showed 15-20% greater decrease in systolic blood pressure and increased (by 25%) chance of developing bradycardia.
Methods: PRISMA guidelines was followed. PubMed, Embase, and Cochrane Library was searched upto May 2025. Eligible studies evaluated pharmacokinetic interactions between β-blockers and CYP2D6-inhibiting SSRIs, duloxetine, or bupropion in adults aged >20 years. Data on drug plasma concentrations, clearance, area under the curve (AUC) were extracted. Statistical analyses conducted using RevMan 5.4, with pooled effect estimates calculated via random-effects models. Heterogeneity assessed using I2 statistics to quantify degree of variability.
Results: Meta-analysis of 65 participants demonstrated pharmacokinetic interactions between beta-blockers and antidepressant medications. S-enantiomers of beta-blockers with SSRIs, AUC increased by 2.55 (95% CI: 1.50–4.34), Cmax by 1.94 (95% CI: 1.48–2.54), half-life by 1.94 (95% CI: 1.62–2.33), with no Tmax change. Heterogeneity was moderate- high for AUC (I2 = 70–77%) and low for Cmax/half-life (I2 = 0%).
Nebivolol with antidepressants, AUC increased by 2.76 (95% CI: 1.47–5.18), Cmax by 1.67 (95% CI: 1.14–2.44), half-life by 1.80 (95% CI: 1.15–2.81). OH-Nebivolol metabolite exhibited greater effects: AUC by 2.59 (95% CI: 1.29–5.20), Cmax by 1.48 (95% CI: 1.32–1.66), half-life by 2.15 (95% CI: 1.28–3.62). Tmax showed no differences. Analysis revealed heterogeneity moderate- high (I2 = 64–86%), except Cmax of metabolite (I2 = 0%).
Conclusion: CYP2D6-metabolized beta-blockers (e.g., metoprolol, carvedilol) are altered by concomitant SSRI/ antidepressant use, increasing systemic exposure, higher plasma levels, and prolonged half-life, potentially intensifying therapeutic and adverse effects. In contrast, beta-blockers (atenolol and nadolol), remain unaffected. Clinicians should assess drug interactions, dose adjustments, and implement monitoring to ensure optimal outcomes.
More abstracts on this topic:
2-Methoxyestradiol By Inhibiting Central Action of 12S-Hydroxyeicosatetraenoic Acid Protects Ovariectomized Mice From Hypertension
Dutta Shubha, Singh Purnima, Song Chi Young, Shin Ji Soo, Malik Kafait
A Blood(y) Pressure Crisis: Diffuse Alveolar Hemorrhage as a Rare Manifestation of Severely Uncontrolled HypertensionNandyal Shreyas, Amdetsion Gedion Yilma, Varma Revati, Kohli Saksham, Hammo Hasan