Final ID: TH208
Evaluating The Accuracy Of Cuffless Devices In Ambulatory Blood Pressure Monitoring: A Systematic Review And Meta-Analysis
Abstract Body: Introduction:
Hypertension is an important modifiable risk factor for cardiovascular diseases. Cuffless blood pressure monitors (CL-BPMs) have emerged as convenient alternatives to traditional cuff-based monitors (C-BPMs). We aim to compare both modalities quantitatively and elaborate on the diagnostic accuracy of CL-BPM. We also discuss the need to address shortcomings of CL-BPMs that limit their current use in widespread clinical practice.
Methods:
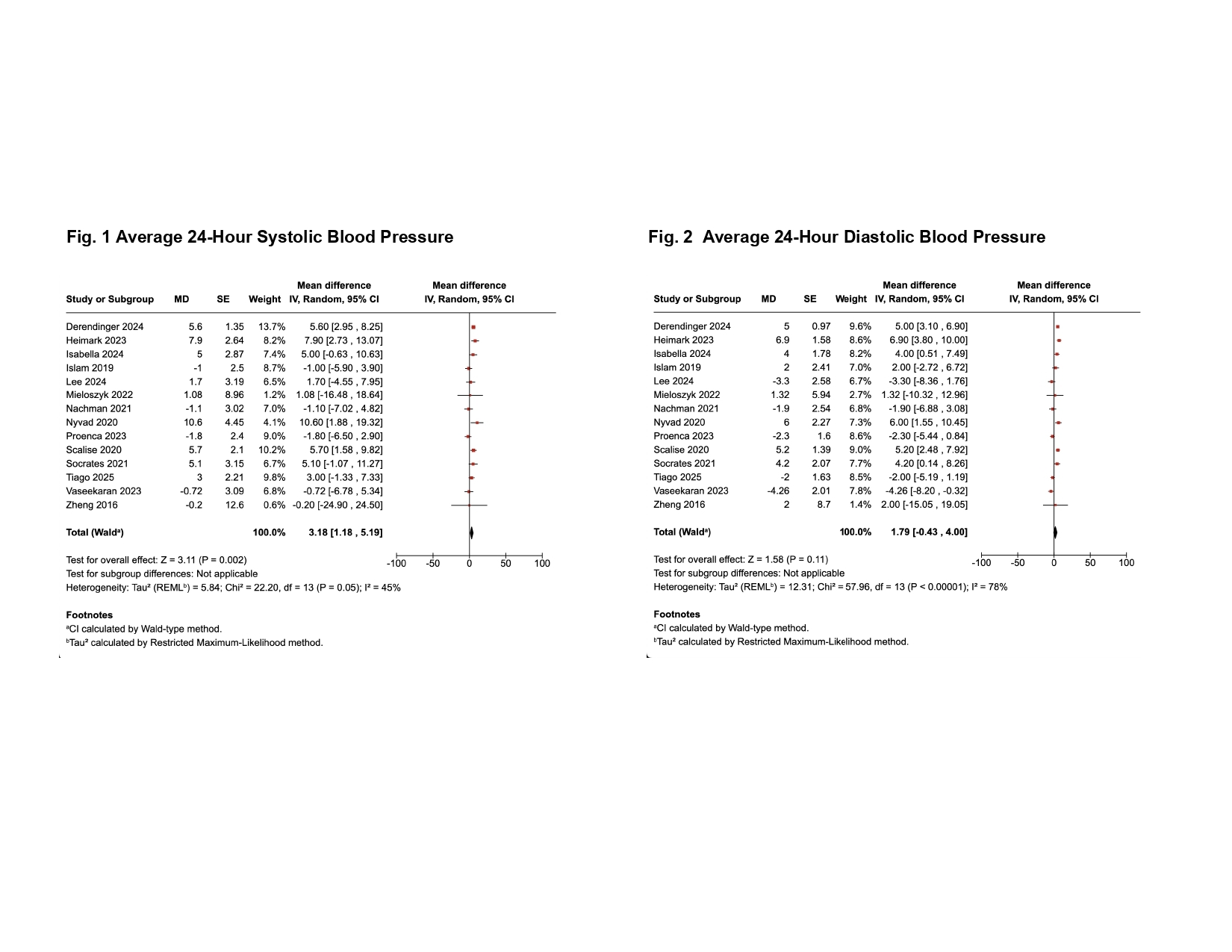
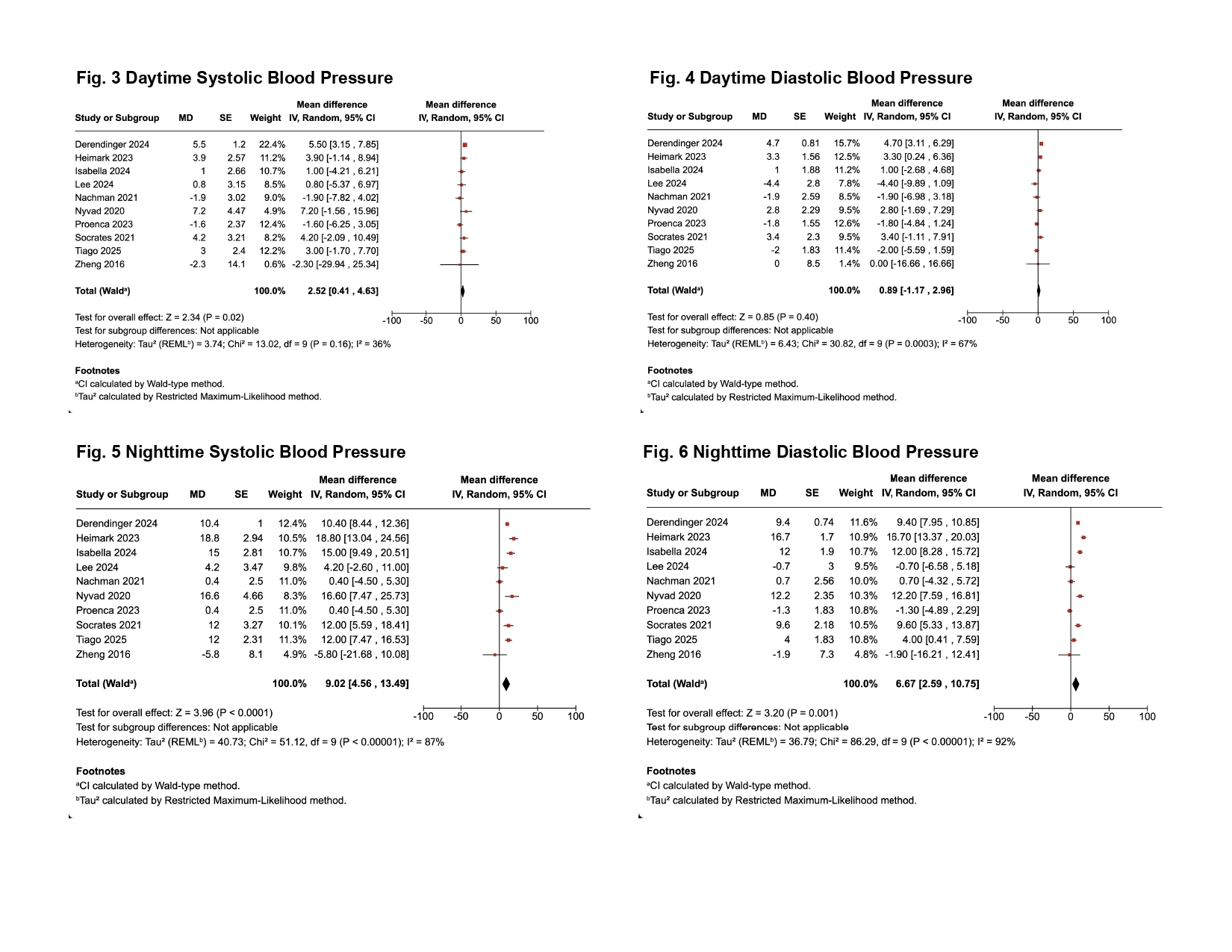
We pooled data from 14 studies that simultaneously compared CL-BPM and C-BPM for ambulatory blood pressure monitoring (ABPM). The results were reported as mean differences (MD) in systolic and diastolic blood pressures (SBP and DBP) between the two modalities. Inverse variance weighted analysis was used to calculate pooled estimates. Tau2 and I2 statistics were used to assess heterogeneity.
Results:
A total of 1011 participants were included. Meta-analysis showed a 24-hour MD of 3.18 [95% CI 1.18-5.19, P=0.002] for SBP and 1.79 [95% CI (-0.43)-4, P=0.11] for DBP, with moderate and high heterogeneity (I2 = 45% and 78%), respectively. MD in daytime SBP and DBP between the two modalities were 2.52 [95% CI 0.41-4.63, P=0.02] and 0.89 [95% CI (-1.17)-2.96, P=0.4], respectively. An MD of 9.02 [95% CI 4.56-13.49, P<0.0001] was observed for nighttime SBP, whereas it was 6.67 [95% CI 2.59-10.75, P=0.001] for nighttime DBP. Our findings suggest a significant difference in means of 24h SPB, day SBP, night SBP, and DBP between the two modalities, suggesting that cuffless monitors are not on par with cuffed monitors for these measurements. However, there was no significant difference in the means of 24-hour DBP and daytime DBP between the two modalities, suggesting that the cuffless devices were as accurate as the cuffed monitors in these scenarios.
Conclusion :
CL-BPMs showed an overall significant MD in BP compared to the standard C-BPM. Although the CL-BPM may be convenient, user-friendly, and help eliminate limb-circumference-based cuff sizing, it has some challenges. These include complex calibration protocols; accuracy concerns in several subgroups like individuals with dark skin tone, obesity, and pregnancy; and inability to track BP during sleep, exercise, and while on antihypertensives. Substantial heterogeneity in the results indicates a lack of standardized validation protocols. Detailed studies and subgroup analyses are required to validate these devices before their widespread use in clinical practice.
Hypertension is an important modifiable risk factor for cardiovascular diseases. Cuffless blood pressure monitors (CL-BPMs) have emerged as convenient alternatives to traditional cuff-based monitors (C-BPMs). We aim to compare both modalities quantitatively and elaborate on the diagnostic accuracy of CL-BPM. We also discuss the need to address shortcomings of CL-BPMs that limit their current use in widespread clinical practice.
Methods:
We pooled data from 14 studies that simultaneously compared CL-BPM and C-BPM for ambulatory blood pressure monitoring (ABPM). The results were reported as mean differences (MD) in systolic and diastolic blood pressures (SBP and DBP) between the two modalities. Inverse variance weighted analysis was used to calculate pooled estimates. Tau2 and I2 statistics were used to assess heterogeneity.
Results:
A total of 1011 participants were included. Meta-analysis showed a 24-hour MD of 3.18 [95% CI 1.18-5.19, P=0.002] for SBP and 1.79 [95% CI (-0.43)-4, P=0.11] for DBP, with moderate and high heterogeneity (I2 = 45% and 78%), respectively. MD in daytime SBP and DBP between the two modalities were 2.52 [95% CI 0.41-4.63, P=0.02] and 0.89 [95% CI (-1.17)-2.96, P=0.4], respectively. An MD of 9.02 [95% CI 4.56-13.49, P<0.0001] was observed for nighttime SBP, whereas it was 6.67 [95% CI 2.59-10.75, P=0.001] for nighttime DBP. Our findings suggest a significant difference in means of 24h SPB, day SBP, night SBP, and DBP between the two modalities, suggesting that cuffless monitors are not on par with cuffed monitors for these measurements. However, there was no significant difference in the means of 24-hour DBP and daytime DBP between the two modalities, suggesting that the cuffless devices were as accurate as the cuffed monitors in these scenarios.
Conclusion :
CL-BPMs showed an overall significant MD in BP compared to the standard C-BPM. Although the CL-BPM may be convenient, user-friendly, and help eliminate limb-circumference-based cuff sizing, it has some challenges. These include complex calibration protocols; accuracy concerns in several subgroups like individuals with dark skin tone, obesity, and pregnancy; and inability to track BP during sleep, exercise, and while on antihypertensives. Substantial heterogeneity in the results indicates a lack of standardized validation protocols. Detailed studies and subgroup analyses are required to validate these devices before their widespread use in clinical practice.
More abstracts on this topic:
Bedtime Versus Morning Dosing of Antihypertensives: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Rakab Mohamed, Abuelazm Mohamed, Elsalakawi Basel Hatem, Mattar Mohab, Shubietah Abdalhakim, Khan Ubaid, Maamoun Alaa, Manasrah Almothana, Elgendy Mohamed, Ruzieh Mohammed
Association Between Antihypertensive Polypharmacy and Midlife Cognitive Function: Insights from the Bogalusa Heart StudyPaul Trishita, Fonseca Lomeli Vanessa, Libon David, Bazzano Lydia, De Anda-duran Ileana