Final ID: MP2181
Association Between Antihypertensive Polypharmacy and Midlife Cognitive Function: Insights from the Bogalusa Heart Study
Abstract Body (Do not enter title and authors here): Introduction: While hypertension is a well-established risk factor for cognitive decline, the relationship between the number of antihypertensive medications (AHMs) used and cognitive function remains unclear. Understanding this association in midlife could improve risk stratification and increase early intervention prior to irreversible cognitive decline. However, few studies have specifically evaluated this relationship in midlife.
Hypothesis: A higher number of concurrently used AHMs is associated with lower midlife cognitive performance, independent of blood pressure control, diabetes treatment, and educational quality.
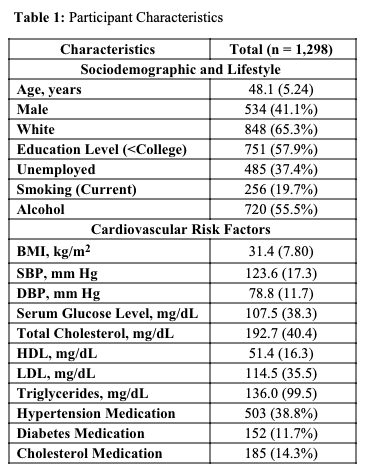
Methods: A total of 1,298 participants (mean age: 48.1 ± 5.24 years; 41% male; 65% White) from the Bogalusa Heart Study who reported prescribed medications and completed neuropsychological testing were included. Cognitive function was assessed using a global cognitive z-score (GCS) derived from nine neuropsychological tests, standardized for age, sex, and race. The primary exposure was the number of AHMs used at the time of cognitive assessment. Multivariable linear regression models were used to evaluate the association between number of AHMs and GCS, further adjusting for hypertension diagnosis, systolic blood pressure, diabetes medication use, and quality of education.
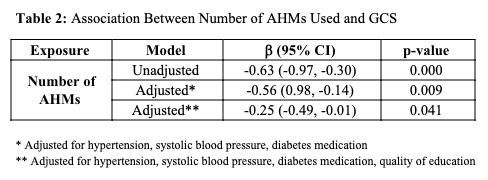
Results: In unadjusted models, each additional AHM used was associated with lower GCS (β = -0.63, 95% CI: -0.97, -0.30; p<0.001). This association remained significant after adjustment for hypertension, systolic blood pressure, and diabetes medication use (β = -0.56, 95% CI: -0.98, -0.14; p=0.009). After further adjustment for educational quality, the association persisted but was attenuated (β = -0.25, 95% CI: -0.49, -0.01; p=0.041).
Conclusion: A higher number of AHMs used was associated with lower midlife cognitive performance, even after accounting for hypertension, blood pressure control, diabetes treatment, and achieved education among other variables. These findings highlight the need for further research to determine whether the number of medications reflects more severe hypertension, a greater burden of comorbidities or complications, or whether polypharmacy itself may directly contribute to cognitive impairment. Longitudinal studies are also warranted to further clarify the relationship between AHM burden and cognition.
Hypothesis: A higher number of concurrently used AHMs is associated with lower midlife cognitive performance, independent of blood pressure control, diabetes treatment, and educational quality.
Methods: A total of 1,298 participants (mean age: 48.1 ± 5.24 years; 41% male; 65% White) from the Bogalusa Heart Study who reported prescribed medications and completed neuropsychological testing were included. Cognitive function was assessed using a global cognitive z-score (GCS) derived from nine neuropsychological tests, standardized for age, sex, and race. The primary exposure was the number of AHMs used at the time of cognitive assessment. Multivariable linear regression models were used to evaluate the association between number of AHMs and GCS, further adjusting for hypertension diagnosis, systolic blood pressure, diabetes medication use, and quality of education.
Results: In unadjusted models, each additional AHM used was associated with lower GCS (β = -0.63, 95% CI: -0.97, -0.30; p<0.001). This association remained significant after adjustment for hypertension, systolic blood pressure, and diabetes medication use (β = -0.56, 95% CI: -0.98, -0.14; p=0.009). After further adjustment for educational quality, the association persisted but was attenuated (β = -0.25, 95% CI: -0.49, -0.01; p=0.041).
Conclusion: A higher number of AHMs used was associated with lower midlife cognitive performance, even after accounting for hypertension, blood pressure control, diabetes treatment, and achieved education among other variables. These findings highlight the need for further research to determine whether the number of medications reflects more severe hypertension, a greater burden of comorbidities or complications, or whether polypharmacy itself may directly contribute to cognitive impairment. Longitudinal studies are also warranted to further clarify the relationship between AHM burden and cognition.
More abstracts on this topic:
Atrial Fibrillation and Risk of Incident Cognitive Impairment: The Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study
Le Vinh, Wilkinson Katherine, Judd Suzanne, Soliman Elsayed, Hyacinth Hyacinth I., Olson Nels, Smith Melissa, Cushman Mary
Association of Cardiopulmonary Resuscitation Strategies with Diffuse Optical Measurements of Cerebral HemodynamicsAnderson Darci, Gaudio Hunter, Morton Sarah, Menezes Forti Rodrigo, Baker Wesley, Kilbaugh Todd, Morgan Ryan, Ko Tiffany, Herrmann Jeremy, Senthil Kumaran, Crozier Aidan, Mason Mckenna, Seeney Alyssa, Ranieri Nicolina, Goto Rika, Krishna Akshatha