Final ID: MDP141
Burden and Impact of Pulmonary Embolism in Young Adults Hospitalized With Sarcoidosis - Underreported Data from Nationwide Analysis (2016-2020)
Abstract Body (Do not enter title and authors here): BACKGROUND:
Studies in the past have demonstrated an association between sarcoidosis and pulmonary embolism but little is known about its impact, especially in young adults. We aim to determine the burden and impact of pulmonary embolism (PE) in young adults hospitalized with sarcoidosis.
METHOD:
The study investigates the prevalence and consequences of PE in young adults aged 18-44 years hospitalized with sarcoidosis using data from the National Inpatient Sample (2016-2020) with relevant ICD-10 codes. This study aims to address the primary outcomes of the burden and trends of PE and its associated impact on in-hospital mortality. Additionally, it explores secondary outcomes such as healthcare resource utilization and discharge patterns.
RESULT:
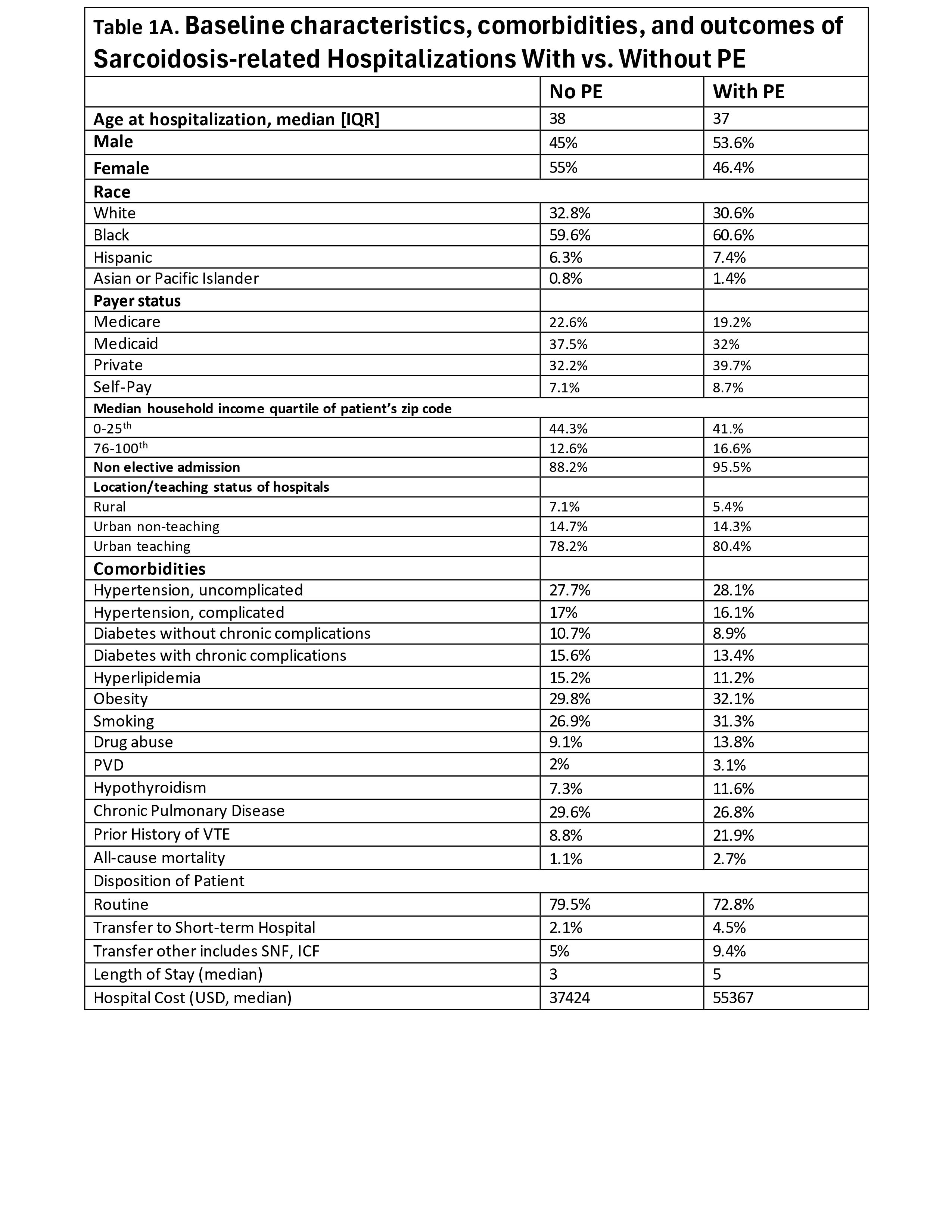
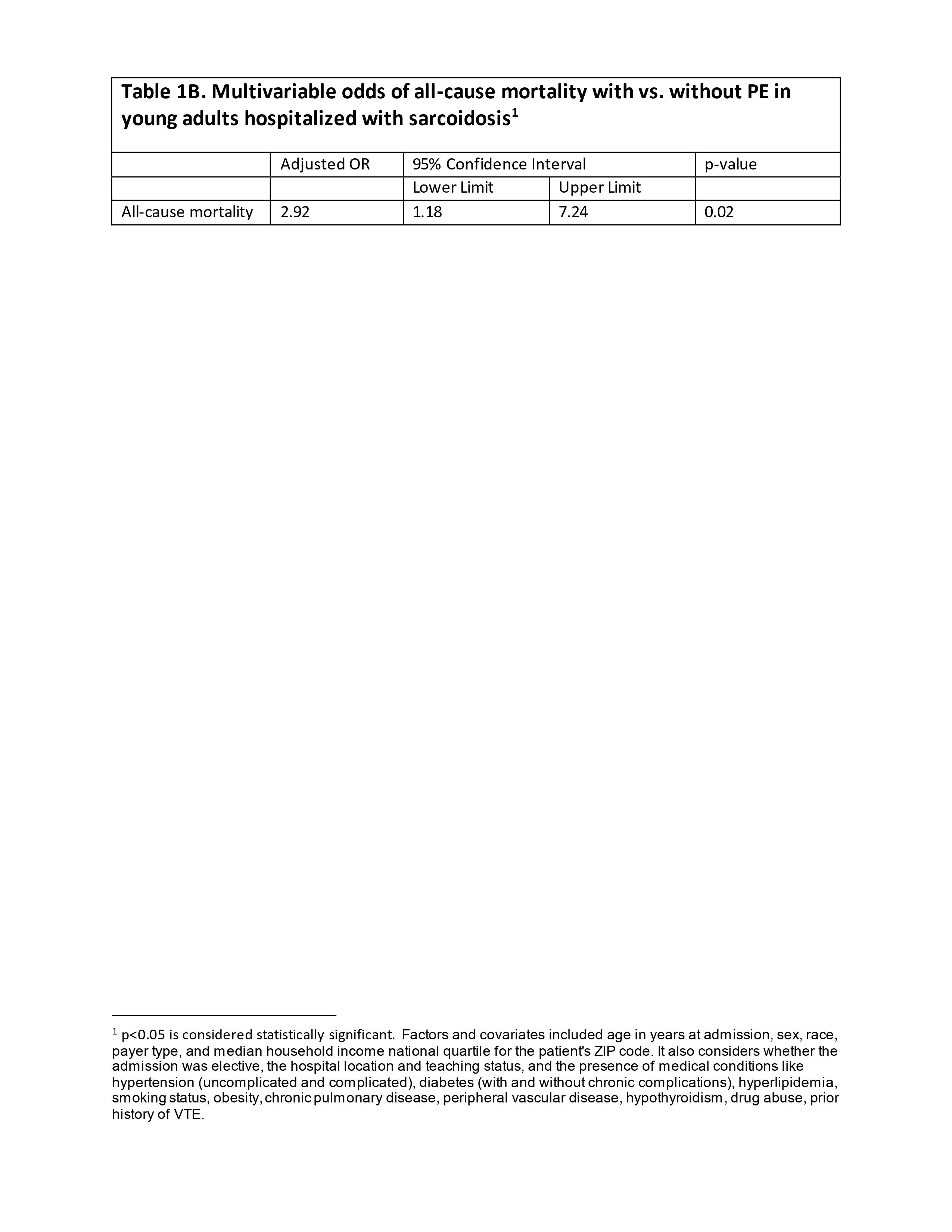
Among 50,385 young adults (median age 37 years) hospitalized with sarcoidosis, 1120 had PE, showing a linear increase from 2% in 2016 to 2.9% (p<0.001) in 2020. Sarcoidosis-PE+ group, predominantly in young blacks, exhibited a higher prevalence of comorbidities such as obesity, smoking, drug use, peripheral vascular disease, hypothyroidism, and prior history of VTE. In contrast, the sarcoidosis-PE- group had a higher prevalence of diabetes (with/without chronic complication), hyperlipidemia, and chronic pulmonary disease. Multivariable regression analysis adjusted for all potential sociodemographic and comorbid variables showed higher odds of all-cause mortality (OR: 2.92, 95% CI: 1.18-7.24, p <0.02) in the sarcoidosis-PE+ group as compared to sarcoidosis-PE- group. The sarcoidosis-PE+ group also had higher hospital costs and length of stay.
CONCLUSION:
The higher odds of in-hospital mortality with an increased length of stay and hospital cost observed in the sarcoidosis-PE+ group highlight the often underreported complications of sarcoidosis, particularly in a younger demographic. The relevance of this study stems from its potential to uncover trends that could lead to improved diagnostic and therapeutic strategies.
Studies in the past have demonstrated an association between sarcoidosis and pulmonary embolism but little is known about its impact, especially in young adults. We aim to determine the burden and impact of pulmonary embolism (PE) in young adults hospitalized with sarcoidosis.
METHOD:
The study investigates the prevalence and consequences of PE in young adults aged 18-44 years hospitalized with sarcoidosis using data from the National Inpatient Sample (2016-2020) with relevant ICD-10 codes. This study aims to address the primary outcomes of the burden and trends of PE and its associated impact on in-hospital mortality. Additionally, it explores secondary outcomes such as healthcare resource utilization and discharge patterns.
RESULT:
Among 50,385 young adults (median age 37 years) hospitalized with sarcoidosis, 1120 had PE, showing a linear increase from 2% in 2016 to 2.9% (p<0.001) in 2020. Sarcoidosis-PE+ group, predominantly in young blacks, exhibited a higher prevalence of comorbidities such as obesity, smoking, drug use, peripheral vascular disease, hypothyroidism, and prior history of VTE. In contrast, the sarcoidosis-PE- group had a higher prevalence of diabetes (with/without chronic complication), hyperlipidemia, and chronic pulmonary disease. Multivariable regression analysis adjusted for all potential sociodemographic and comorbid variables showed higher odds of all-cause mortality (OR: 2.92, 95% CI: 1.18-7.24, p <0.02) in the sarcoidosis-PE+ group as compared to sarcoidosis-PE- group. The sarcoidosis-PE+ group also had higher hospital costs and length of stay.
CONCLUSION:
The higher odds of in-hospital mortality with an increased length of stay and hospital cost observed in the sarcoidosis-PE+ group highlight the often underreported complications of sarcoidosis, particularly in a younger demographic. The relevance of this study stems from its potential to uncover trends that could lead to improved diagnostic and therapeutic strategies.
More abstracts on this topic:
A Case Report: Outpatient Diagnosis of Venous Stent Migration - Avoiding Catastrophic Outcomes
Basnyat Anouksha, Pamganamamula Madhu, Naidu Raja, Pamganamamula Teja, Manchiraju Srinidhi, Gaddam Srilakshmi, Panganamamula Lalitha
A Rare Case of Atypical Sarcoidosis Presenting as an Intra-Atrial Septal MassDod Rohan, Tushak Zackary