Final ID: FR500
Gender, Racial, and Geographic Trends and Disparities in Mortality Due to Aortic Aneurysm and Dissection with Hypertension in Adults Aged 25 and Older in the United States
Abstract Body: Introduction: Hypertension is a major contributor to aortic aneurysm and dissection, conditions with high mortality. Despite this, national trends in hypertension-related deaths involving aortic aneurysm and dissection remain poorly characterized.
Hypothesis: We hypothesized that mortality from hypertension associated aortic aneurysm and dissection has changed over time and that significant disparities exist across race, sex, and geographic regions in the United States from 1999 to 2020.
Methods: We retrospectively analyzed CDC WONDER mortality data for US adults aged 25 years and older from 1999 to 2020. Deaths were included if both hypertension (ICD-10: I10–I15) and aortic aneurysm and dissection (ICD-10: I71) were listed on the death certificate. Joinpoint regression was used to estimate annual percent change (APC) and average annual percent change (AAPC). Age-adjusted mortality rates (AAMRs) per 100,000 persons were calculated, stratified by year, sex, race, age group, and geographical region.
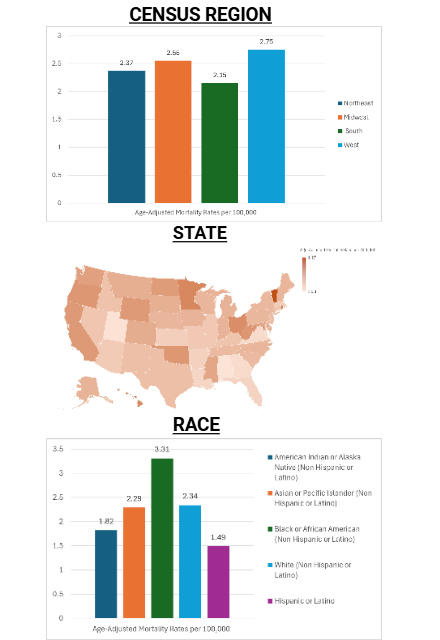
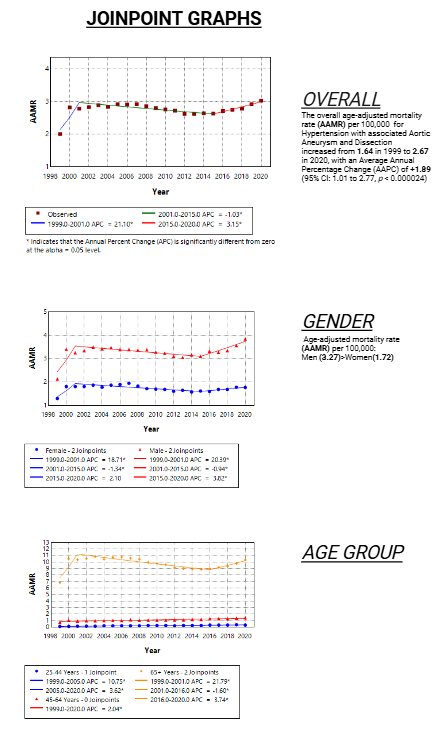
Results: From 1999 to 2020, 113,728 deaths were recorded due to hypertension-associated aortic aneurysm and dissection among adults aged ≥25 in the US. The overall AAMR increased from 1.64 in 1999 to 2.67 in 2020, with an AAPC of +1.89 (95% CI: 1.01 to 2.77, p < 0.000024). Men had higher overall AAMRs (3.27) compared to women (1.72), with a more significant increase in men (AAPC: +2.05, p < 0.000001) than in women (AAPC: +1.23, p < 0.049). Racial disparities showed the highest AAMRs in non-Hispanic (NH) Blacks (3.31), followed by NH Whites (2.34), NH Asian/Pacific Islanders (2.29), NH American Indian/Alaska Natives (1.82), and Hispanic adults (1.49). Among age groups, the most significant increase was observed in adults aged 25 to 44 years (AAPC: +5.6, p < 0.000001) compared to those 45 to 65 and 65 above. Geographically, AAMRs ranged from 1.53 in Alabama to 4.47 in Vermont, with the highest mortality observed in the Western region (AAMR: 2.75). Nonmetropolitan areas exhibited slightly higher AAMRs (2.46) than metropolitan areas (2.40).
Conclusion:
Mortality from hypertension-related aortic aneurysm and dissection has increased nationally, with higher rates among men, NH Black adults, and younger individuals. These disparities highlight the need for targeted public health strategies to ensure equitable access to care. Further work is needed to better understand and address the fundamental factors driving these disparities.
Hypothesis: We hypothesized that mortality from hypertension associated aortic aneurysm and dissection has changed over time and that significant disparities exist across race, sex, and geographic regions in the United States from 1999 to 2020.
Methods: We retrospectively analyzed CDC WONDER mortality data for US adults aged 25 years and older from 1999 to 2020. Deaths were included if both hypertension (ICD-10: I10–I15) and aortic aneurysm and dissection (ICD-10: I71) were listed on the death certificate. Joinpoint regression was used to estimate annual percent change (APC) and average annual percent change (AAPC). Age-adjusted mortality rates (AAMRs) per 100,000 persons were calculated, stratified by year, sex, race, age group, and geographical region.
Results: From 1999 to 2020, 113,728 deaths were recorded due to hypertension-associated aortic aneurysm and dissection among adults aged ≥25 in the US. The overall AAMR increased from 1.64 in 1999 to 2.67 in 2020, with an AAPC of +1.89 (95% CI: 1.01 to 2.77, p < 0.000024). Men had higher overall AAMRs (3.27) compared to women (1.72), with a more significant increase in men (AAPC: +2.05, p < 0.000001) than in women (AAPC: +1.23, p < 0.049). Racial disparities showed the highest AAMRs in non-Hispanic (NH) Blacks (3.31), followed by NH Whites (2.34), NH Asian/Pacific Islanders (2.29), NH American Indian/Alaska Natives (1.82), and Hispanic adults (1.49). Among age groups, the most significant increase was observed in adults aged 25 to 44 years (AAPC: +5.6, p < 0.000001) compared to those 45 to 65 and 65 above. Geographically, AAMRs ranged from 1.53 in Alabama to 4.47 in Vermont, with the highest mortality observed in the Western region (AAMR: 2.75). Nonmetropolitan areas exhibited slightly higher AAMRs (2.46) than metropolitan areas (2.40).
Conclusion:
Mortality from hypertension-related aortic aneurysm and dissection has increased nationally, with higher rates among men, NH Black adults, and younger individuals. These disparities highlight the need for targeted public health strategies to ensure equitable access to care. Further work is needed to better understand and address the fundamental factors driving these disparities.
More abstracts on this topic:
A Meta-Analysis of Prospective Studies Comparing Short and Longterm Outcomes of Trans-Catheter Aortic Valve Replacement in Patient with and without Cancer:
Khan Muhammad Aslam, Haider Adnan, Haider Taimoor, Bhattarai Shraddha, Khan Bilal, Lamichhane Bikal, Shafique Nouman, Rahman Hammad, Aafreen Asna, Muhammad Anza, Bhatia Hitesh, Khan Abid Nawaz Khan, Akbar Usman, Khan Alamzaib
Achieving Guidelines within a 24-Hour Movement Paradigm and Risk of Cardiovascular Disease and All-Cause Mortality in United States AdultsBoudreaux Benjamin, Xu Chang, Dooley Erin, Hornikel Bjoern, Munson Alexandra, Shechter Ari, Palta Priya, Gabriel Kelley, Diaz Keith