Final ID: TAC134
Impact of Mediterranean Diet on Hypertension in Patients with High Cardiovascular disease Risk: A Systematic Review & Meta-Analysis of Randomized Controlled Trials
Abstract Body: Introduction:
The rising global burden of hypertension necessitates the identification of effective strategies for its control and prevention, complementing advancements in pharmacotherapy. The Mediterranean diet (MedDiet), characterized by high intake of fruits, vegetables, whole grains, nuts, legumes, and olive oil, with moderate fish and wine consumption, has demonstrated cardiovascular benefits, including reduction in blood pressure. However, the impact of MedDiet on hypertension in patients with high cardiovascular disease (CVD) risk remains understudied. This systematic review and meta-analysis aim to evaluate the impact of the MedDiet on blood pressure (BP) in patients at high CVD risk.
Methods:
A systematic literature search was conducted across PubMed/MEDLINE, Scopus, Science Direct, Cochrane/CENTRAL, and clinical trial registries (clinicaltrials.gov), adhering to PRISMA guidelines. RCTs (Randomized Controlled Trials) reporting the effect of MedDiet on systolic (SBP) and diastolic (DBP) blood pressure in adults with pre-existing CVD or multiple CVD risk factors were included in the study. Random-effects models with inverse variance weighting were used to calculate weighted mean differences (WMDs) with 95% confidence intervals (CIs) for changes in SBP and DBP. Meta-analysis was conducted using the R-metafor package. A p-value ≤0.05 was considered statistically significant.
Results:
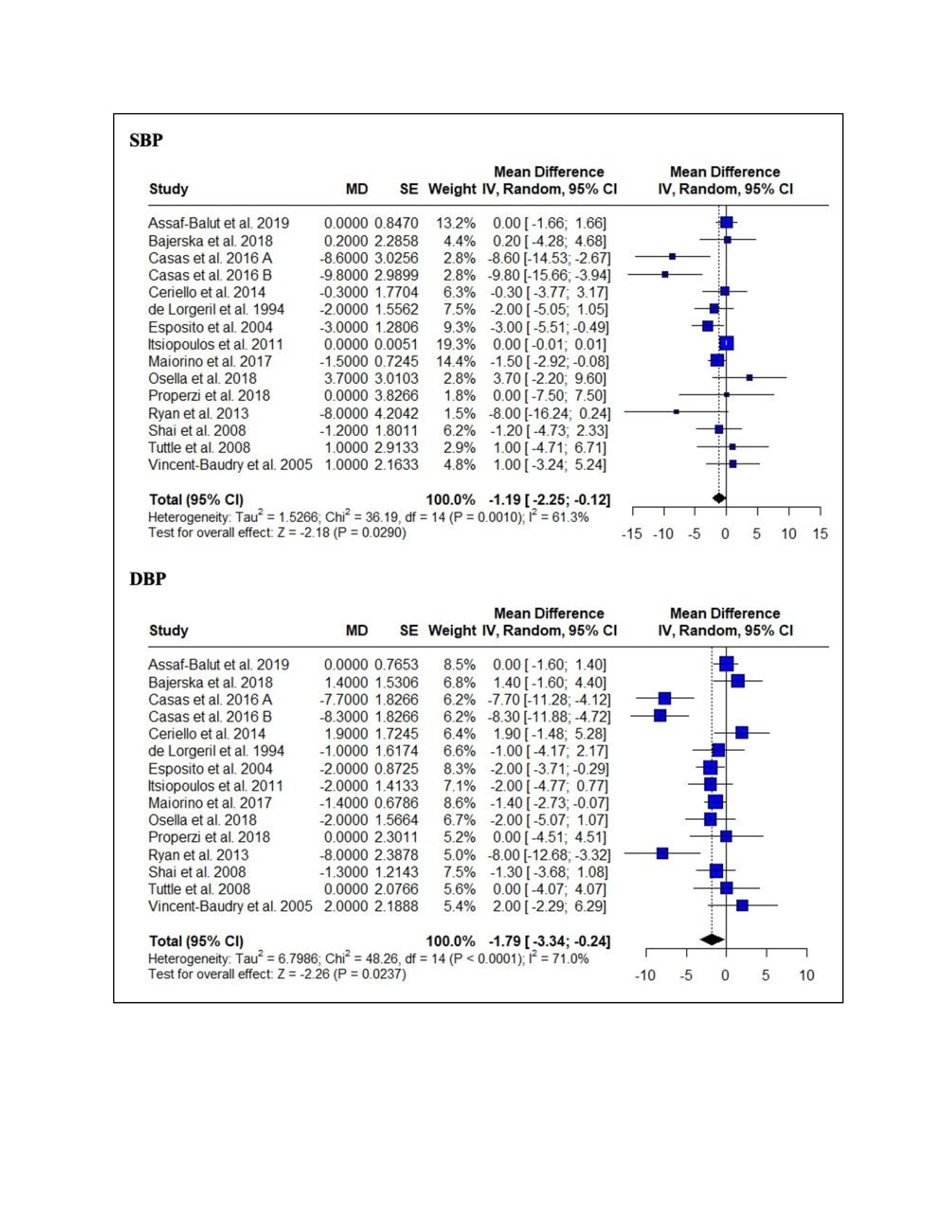
A total of 14 RCTs encompassing 2,698 patients (50.8% males) with high CVD risk are included in the analysis. The MedDiet group had a significant reduction of SBP [SMD -1.19; 95% CI 2.25; -0.12; p=0.03] and DBP [-1.79; 95% CI -3.34; -0.24; p=0.02] compared to the control group (Figure 1).
Conclusion:
MedDiet significantly reduces both SBP and DBP in patients at high risk of CVD, underscoring the clinical importance of MedDiet as a potent non-pharmacological intervention for hypertension management and CVD prevention in this vulnerable population. Future research should focus on elucidating optimal strategies for long-term adherence to the MedDiet, exploring the specific dietary components that contribute most to blood pressure reduction, and assessing the cost-effectiveness of MedDiet interventions in diverse healthcare settings.
The rising global burden of hypertension necessitates the identification of effective strategies for its control and prevention, complementing advancements in pharmacotherapy. The Mediterranean diet (MedDiet), characterized by high intake of fruits, vegetables, whole grains, nuts, legumes, and olive oil, with moderate fish and wine consumption, has demonstrated cardiovascular benefits, including reduction in blood pressure. However, the impact of MedDiet on hypertension in patients with high cardiovascular disease (CVD) risk remains understudied. This systematic review and meta-analysis aim to evaluate the impact of the MedDiet on blood pressure (BP) in patients at high CVD risk.
Methods:
A systematic literature search was conducted across PubMed/MEDLINE, Scopus, Science Direct, Cochrane/CENTRAL, and clinical trial registries (clinicaltrials.gov), adhering to PRISMA guidelines. RCTs (Randomized Controlled Trials) reporting the effect of MedDiet on systolic (SBP) and diastolic (DBP) blood pressure in adults with pre-existing CVD or multiple CVD risk factors were included in the study. Random-effects models with inverse variance weighting were used to calculate weighted mean differences (WMDs) with 95% confidence intervals (CIs) for changes in SBP and DBP. Meta-analysis was conducted using the R-metafor package. A p-value ≤0.05 was considered statistically significant.
Results:
A total of 14 RCTs encompassing 2,698 patients (50.8% males) with high CVD risk are included in the analysis. The MedDiet group had a significant reduction of SBP [SMD -1.19; 95% CI 2.25; -0.12; p=0.03] and DBP [-1.79; 95% CI -3.34; -0.24; p=0.02] compared to the control group (Figure 1).
Conclusion:
MedDiet significantly reduces both SBP and DBP in patients at high risk of CVD, underscoring the clinical importance of MedDiet as a potent non-pharmacological intervention for hypertension management and CVD prevention in this vulnerable population. Future research should focus on elucidating optimal strategies for long-term adherence to the MedDiet, exploring the specific dietary components that contribute most to blood pressure reduction, and assessing the cost-effectiveness of MedDiet interventions in diverse healthcare settings.
More abstracts on this topic:
Association Between Diet Quality, Hypertension, And Hypertension Awareness Among Adults In Puerto Rico
Tamez Martha, Kaplan Robert, Rodriguez-orengo Jose F, Tucker Katherine, Mattei Josiemer
A Blood(y) Pressure Crisis: Diffuse Alveolar Hemorrhage as a Rare Manifestation of Severely Uncontrolled HypertensionNandyal Shreyas, Amdetsion Gedion Yilma, Varma Revati, Kohli Saksham, Hammo Hasan