Final ID: TAC202
Hypertensive Emergency Hospitalizations and Mortality Trends Among Hispanic and Black Populations in the U.S. (2005–2022): An Integrated Analysis of CDC WONDER and National Inpatient Data
Abstract Body: Background
Hypertensive crises are becoming more common, and they disproportionately affect racial and ethnic minorities in the United States. While national databases insights into mortality and hospitalization trends on their own, few studies have combined population-level and clinical data to provide a complete assessment of this growing disaster. This research combines CDC WONDER mortality data with hospitalization outcomes from the National Inpatient Sample (NIS) to look at temporal patterns and disparities among Hispanic and Black individuals from 2005 to 2022.
Methods
Mortality data were obtained from the CDC WONDER Multiple Cause of Death database (ICD-10 codes I10-I16), and hospitalization data from the NIS (2005-2021), with hypertensive emergency admissions identified using ICD-9-CM code 401.0 and ICD-10-CM codes I16.0-I16.9. We calculated age-adjusted mortality rates (AAMRs) per 100,000 people and hospitalization rates by race/ethnicity (Black, Hispanic, and White). In-hospital mortality, extended stay (>4 days), and comorbidity load were among the NIS outcomes. Joinpoint regression identified major inflection points and annual percentage increases (APC).
Results
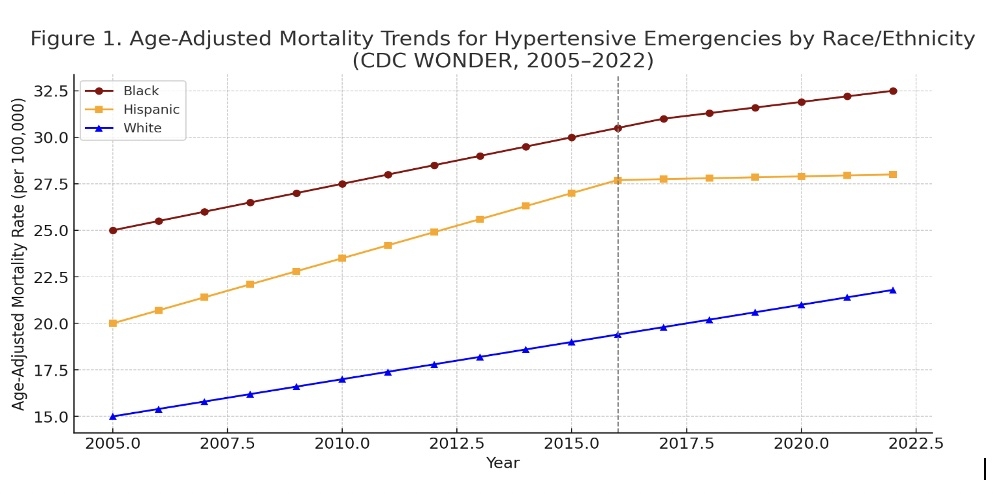
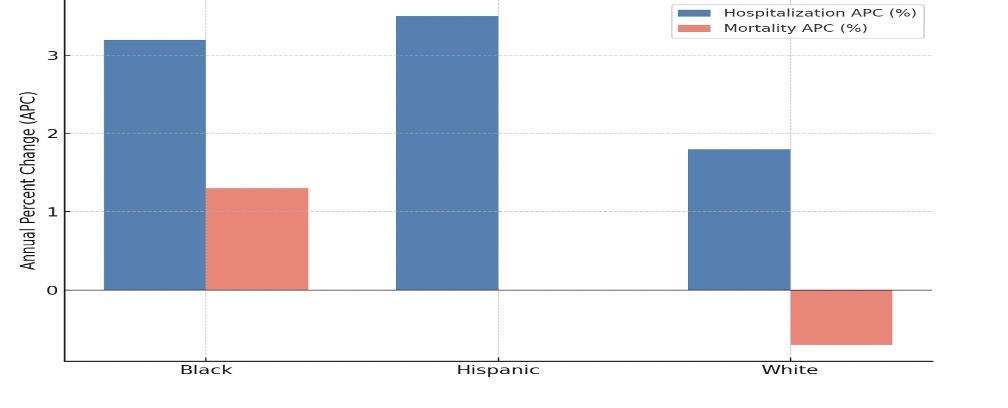
From 2005 to 2022, the CDC reported a 64% increase in hypertensive emergency-related mortality, with the largest increases among Hispanic (+91%) and Black (+78%) groups. AAMRs plateaued for Hispanics after 2016 but increased for Black patients from 2018 to 2022 (APC +1.3%, p = 0.04). A parallel analysis of 1.7 million NIS hospitalizations revealed similar trends: Black individuals were hospitalized at the highest incidence (42.7 per 100,000), followed by Hispanics (33.1) and whites (21.4). Although total in-hospital mortality has decreased, it remains disproportionately high among minority groups, particularly those with chronic renal disease in low-income ZIP locations.
Conclusion
This dual-dataset analysis indicates an increasing and unequal incidence of hypertensive crises in the United States, particularly among Hispanic and Black populations. While clinical results have modestly improved, persistent mortality disparities need for community-based, culturally appropriate hypertension management and upstream public health interventions. Addressing socioeconomic causes, increasing access to treatment, and improving early detection in high-risk groups are critical for reversing these trends.
Hypertensive crises are becoming more common, and they disproportionately affect racial and ethnic minorities in the United States. While national databases insights into mortality and hospitalization trends on their own, few studies have combined population-level and clinical data to provide a complete assessment of this growing disaster. This research combines CDC WONDER mortality data with hospitalization outcomes from the National Inpatient Sample (NIS) to look at temporal patterns and disparities among Hispanic and Black individuals from 2005 to 2022.
Methods
Mortality data were obtained from the CDC WONDER Multiple Cause of Death database (ICD-10 codes I10-I16), and hospitalization data from the NIS (2005-2021), with hypertensive emergency admissions identified using ICD-9-CM code 401.0 and ICD-10-CM codes I16.0-I16.9. We calculated age-adjusted mortality rates (AAMRs) per 100,000 people and hospitalization rates by race/ethnicity (Black, Hispanic, and White). In-hospital mortality, extended stay (>4 days), and comorbidity load were among the NIS outcomes. Joinpoint regression identified major inflection points and annual percentage increases (APC).
Results
From 2005 to 2022, the CDC reported a 64% increase in hypertensive emergency-related mortality, with the largest increases among Hispanic (+91%) and Black (+78%) groups. AAMRs plateaued for Hispanics after 2016 but increased for Black patients from 2018 to 2022 (APC +1.3%, p = 0.04). A parallel analysis of 1.7 million NIS hospitalizations revealed similar trends: Black individuals were hospitalized at the highest incidence (42.7 per 100,000), followed by Hispanics (33.1) and whites (21.4). Although total in-hospital mortality has decreased, it remains disproportionately high among minority groups, particularly those with chronic renal disease in low-income ZIP locations.
Conclusion
This dual-dataset analysis indicates an increasing and unequal incidence of hypertensive crises in the United States, particularly among Hispanic and Black populations. While clinical results have modestly improved, persistent mortality disparities need for community-based, culturally appropriate hypertension management and upstream public health interventions. Addressing socioeconomic causes, increasing access to treatment, and improving early detection in high-risk groups are critical for reversing these trends.
More abstracts on this topic:
BMI Thresholds and Incident ASCVD in Disaggregated Asian American, Native Hawaiian and other Pacific Islander Men and Women: The PANACHE Study
Go Alan, Parikh Rishi, Tan Thida, Ambrosy Andrew, Alexeeff Stacey, Howick Connor, Daida Yihe, Lo Joan
3CPR Best Abstract Award: The pathogenic role of ADAMTS13 deficiency in Chronic Thromboembolic Pulmonary HypertensionWu Zhijian, Zheng X. Long, Zheng Liang