Final ID: FR536
Hypertension-Driven Cardiovascular Mortality Disparities Among U.S. Veterans (1999–2021): A CDC WONDER Analysis
Abstract Body: Background
Veterans in the United States are a medically vulnerable demographic, with an increased risk of heart disease owing to service-related stresses, a high incidence of hypertension, and barriers to preventative care access. Cardiovascular disease (CVD) is the major cause of death in this population; thus, it is critical to monitor long-term mortality patterns, particularly by gender and race, to develop equitable public health initiatives.
Objective
We hypothesized that while overall CVD mortality among U.S. veterans has declined, hypertension-driven disparities by race and sex have persisted or widened over time.
Methods
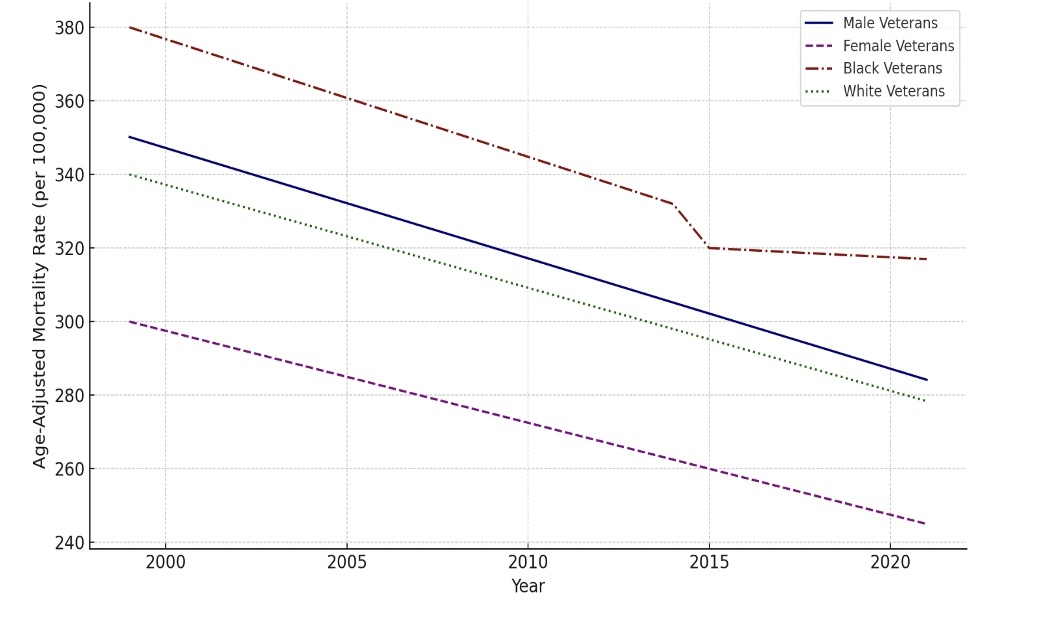
Using ICD-10 codes I00-I99, we examined CDC WONDER mortality data from 1999 to 2021 to identify cardiovascular disease fatalities among veterans aged 25 and older. We used the 2000 US standard population to calculate the age-adjusted mortality rates (AAMRs) per 100,000 people. We examined changes in trajectory over time using subgroup analysis by sex and ethnicity, as well as trend inflection points.
Results
From 1999 to 2021, the AAMR for CVD among veterans decreased by 28.5% (from 350.2 to 250.4 per 100,000). However, the decrease slowed after 2015. In 2021, male veterans had a higher AAMR (270.5) than female veterans (190.3). Racial disparities were significant and persisted: Black veterans had a substantially higher AAMR (300.7) than white veterans (240.1). Despite an overall decline in CVD mortality over the last two decades, these inequalities have remained rather consistent.
Conclusion
Although cardiovascular mortality among U.S. veterans has decreased overall, significant disparities—particularly those attributed to uncontrolled hypertension—remain across gender and race lines. These results targeted hypertension screening, culturally relevant preventative measures, and fair financial allocation at the Veterans Health Administration. Tailored treatments that address both social and clinical factors are critical to reduce avoidable death in this high-risk group.
Veterans in the United States are a medically vulnerable demographic, with an increased risk of heart disease owing to service-related stresses, a high incidence of hypertension, and barriers to preventative care access. Cardiovascular disease (CVD) is the major cause of death in this population; thus, it is critical to monitor long-term mortality patterns, particularly by gender and race, to develop equitable public health initiatives.
Objective
We hypothesized that while overall CVD mortality among U.S. veterans has declined, hypertension-driven disparities by race and sex have persisted or widened over time.
Methods
Using ICD-10 codes I00-I99, we examined CDC WONDER mortality data from 1999 to 2021 to identify cardiovascular disease fatalities among veterans aged 25 and older. We used the 2000 US standard population to calculate the age-adjusted mortality rates (AAMRs) per 100,000 people. We examined changes in trajectory over time using subgroup analysis by sex and ethnicity, as well as trend inflection points.
Results
From 1999 to 2021, the AAMR for CVD among veterans decreased by 28.5% (from 350.2 to 250.4 per 100,000). However, the decrease slowed after 2015. In 2021, male veterans had a higher AAMR (270.5) than female veterans (190.3). Racial disparities were significant and persisted: Black veterans had a substantially higher AAMR (300.7) than white veterans (240.1). Despite an overall decline in CVD mortality over the last two decades, these inequalities have remained rather consistent.
Conclusion
Although cardiovascular mortality among U.S. veterans has decreased overall, significant disparities—particularly those attributed to uncontrolled hypertension—remain across gender and race lines. These results targeted hypertension screening, culturally relevant preventative measures, and fair financial allocation at the Veterans Health Administration. Tailored treatments that address both social and clinical factors are critical to reduce avoidable death in this high-risk group.
More abstracts on this topic:
Ablation vs. Antiarrhythmic Drugs in Atrial Fibrillation: Real-World Treatment Gaps, Outcomes, and Equity Challenges
Rauf Saman, Iqbal Fatima, Bhatti Shehzeen Dua, Masood Natasha, Qureshi Muhammad Maaz, Nawaz Muhammad Hassan
A Key Role of Proximal Tubule Renin-Angiotensin System in The Kidney in The Development of Kidney Ischemia and Reperfusion InjuryLi Xiao, Hassan Rumana, Katsurada Akemi, Sato Ryosuke, Zhuo Jia