Final ID: FR502
Cerebral Perfusion in the Heart-Brain Axis: Cardiovascular Determinants and Association with Subclinical Brain Injury
Abstract Body: Background: Cerebral perfusion is a key component of cerebrovascular integrity, and its impairment with aging may contribute to both cerebrovascular and neurodegenerative disease. However, the interplay between cardiovascular morphology, cerebral hemodynamics, and subclinical brain injury is not well understood.
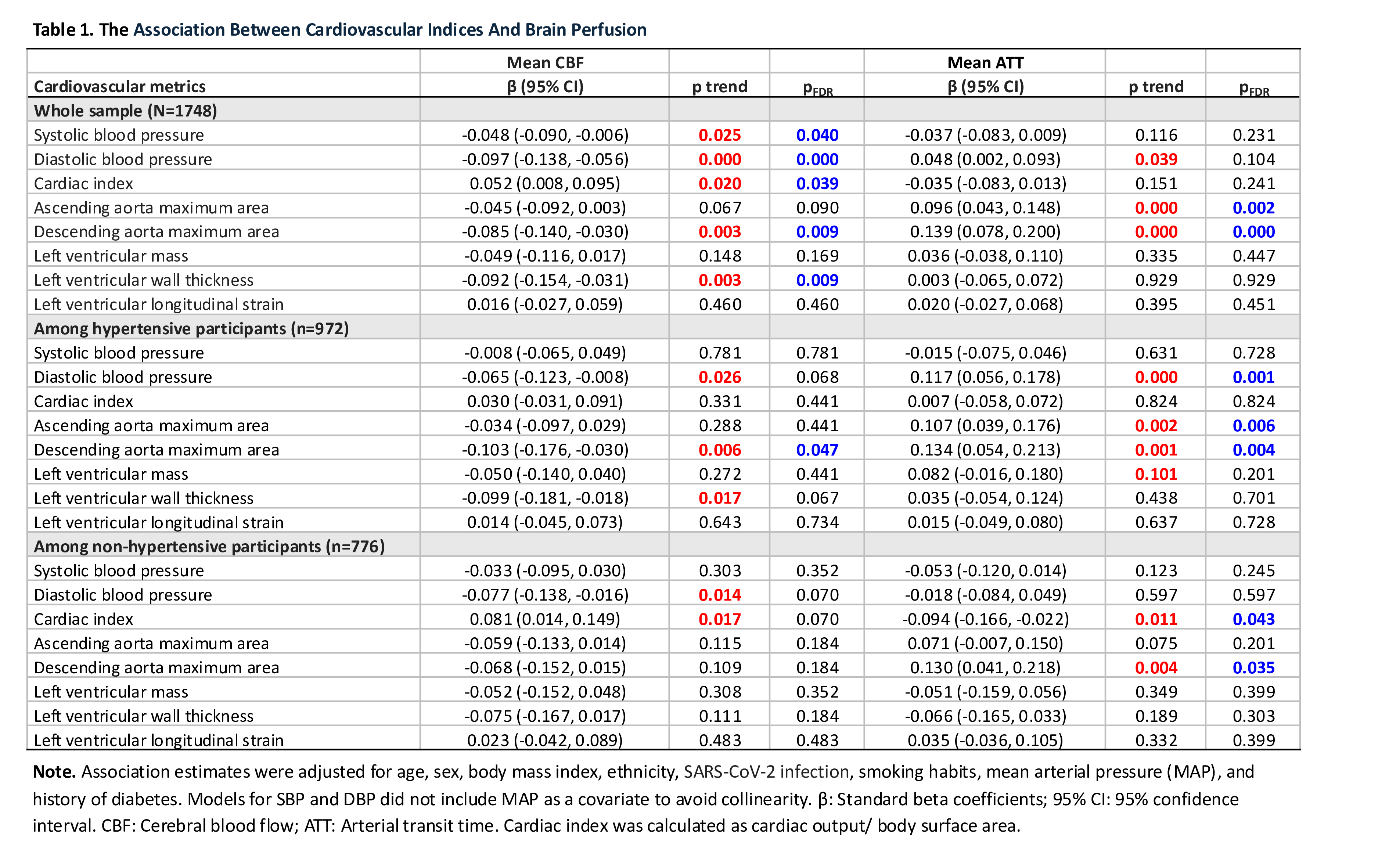
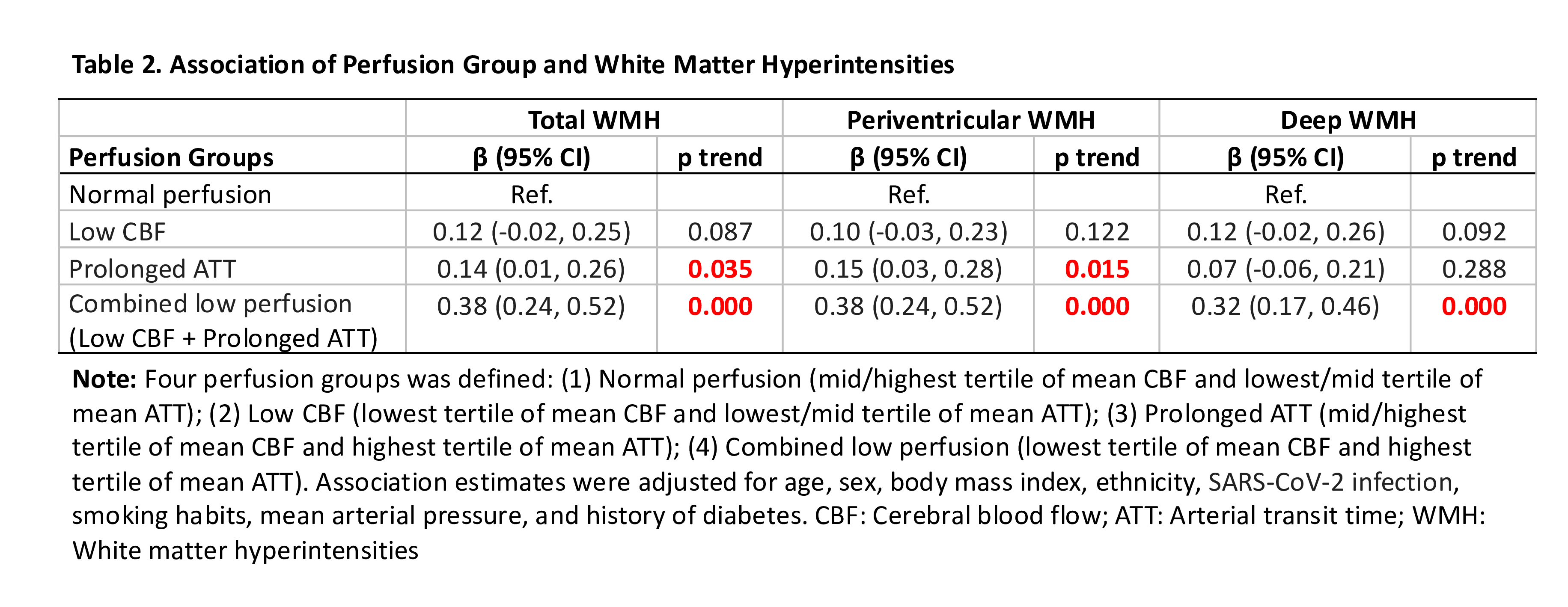
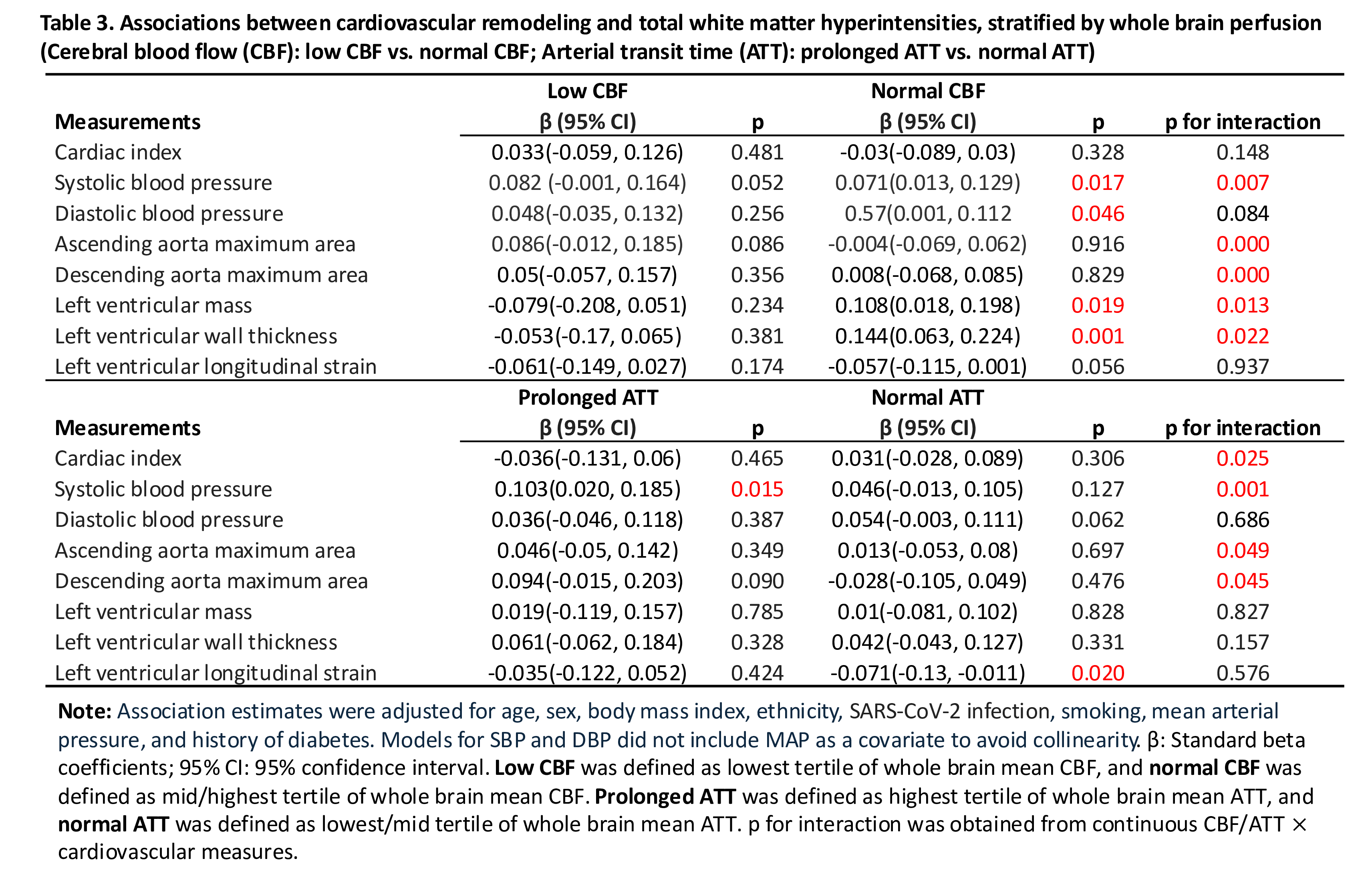
Objective and Methods: We investigated the relationship between cardiovascular indices (measured in 2015), cerebral perfusion metrics, and subclinical brain injury (both measured in 2019) in 1,748 healthy older adults (56.1% women; mean age: 59.8 years) with 1.5T cardiac MRI and multi-modal 3T brain MRI measurements from the UK Biobank study. We assessed eight cardiovascular measures (Table 1). Cerebral perfusion metrics included cerebral blood flow (CBF) and arterial transit time (ATT) and were measured using Arterial Spin Labeling with a multi-post labeling delay protocol. Subclinical brain injury was measured by white matter hyperintensity (WMH) volume from T2 FLAIR images. We examined the association between cardiovascular morphology and brain perfusion and between brain perfusion measures and WMH using multivariable linear models. We further assessed the effect modification by brain perfusion on the relationship between cardiovascular morphology and WMH.
Results: Five cardiovascular measures were significantly associated with lower CBF, both globally and across four cortical regions. Specifically, per standard deviation (SD) decrease in cardiac index was associated with lower CBF (0.052 ml/100g/min; 95% CI: 0.008 to 0.095), while increase in ascending aortic area, LV wall thickness, SBP, and DBP was associated with lower CBF. In contrast, impaired aortic compliance was linked to prolonged ATT (Table 1). Furthermore, lower CBF and longer ATT independently predicted higher WMH burden, with the highest WMH observed in participants with low CBF and prolonged ATT, who showed a 0.37 SD greater burden compared to those with normal perfusion (Table 2). Finally, brain perfusion modified the relationship between cardiovascular morphology and WMH, with a pronounced association observed in those with low CBF or prolonged ATT (p for interaction < 0.05) (Table 3).
Conclusions: Impaired cerebral perfusion may represent a mechanistic pathway linking cardiovascular morphology to white matter injury. Jointly considering CBF and ATT may improve the detection of high-risk individuals with abnormal cerebral perfusion and cerebrovascular vulnerability to brain aging.
Objective and Methods: We investigated the relationship between cardiovascular indices (measured in 2015), cerebral perfusion metrics, and subclinical brain injury (both measured in 2019) in 1,748 healthy older adults (56.1% women; mean age: 59.8 years) with 1.5T cardiac MRI and multi-modal 3T brain MRI measurements from the UK Biobank study. We assessed eight cardiovascular measures (Table 1). Cerebral perfusion metrics included cerebral blood flow (CBF) and arterial transit time (ATT) and were measured using Arterial Spin Labeling with a multi-post labeling delay protocol. Subclinical brain injury was measured by white matter hyperintensity (WMH) volume from T2 FLAIR images. We examined the association between cardiovascular morphology and brain perfusion and between brain perfusion measures and WMH using multivariable linear models. We further assessed the effect modification by brain perfusion on the relationship between cardiovascular morphology and WMH.
Results: Five cardiovascular measures were significantly associated with lower CBF, both globally and across four cortical regions. Specifically, per standard deviation (SD) decrease in cardiac index was associated with lower CBF (0.052 ml/100g/min; 95% CI: 0.008 to 0.095), while increase in ascending aortic area, LV wall thickness, SBP, and DBP was associated with lower CBF. In contrast, impaired aortic compliance was linked to prolonged ATT (Table 1). Furthermore, lower CBF and longer ATT independently predicted higher WMH burden, with the highest WMH observed in participants with low CBF and prolonged ATT, who showed a 0.37 SD greater burden compared to those with normal perfusion (Table 2). Finally, brain perfusion modified the relationship between cardiovascular morphology and WMH, with a pronounced association observed in those with low CBF or prolonged ATT (p for interaction < 0.05) (Table 3).
Conclusions: Impaired cerebral perfusion may represent a mechanistic pathway linking cardiovascular morphology to white matter injury. Jointly considering CBF and ATT may improve the detection of high-risk individuals with abnormal cerebral perfusion and cerebrovascular vulnerability to brain aging.
More abstracts on this topic:
4D Flow MRI Evaluation of Cardiovascular Risk-Related Alterations in Heart-Brain Hemodynamics in Cognitively Healthy Aging Adults
Najafi Anahita, Rogalski Emily, Jarvis Kelly, Richter Adam, Lytchakov Anna, Benson Theresa, Jin Ning, Davids Rachel, Schnell Susanne, Ragin Ann, Weintraub Sandra
A Culturally Tailored mHealth Lifestyle Intervention Improves Diet and Physical Activity Self-Regulation Among African AmericansLalika Mathias, Jenkins Sarah, Hayes Sharonne, Jones Clarence, Burke Lora, Cooper Lisa, Patten Christi, Brewer Laprincess