Final ID: TH214
Associations between 24-hour Blood Pressure Variability Measures and Orthostatic Blood Pressure Changes
Objective: To examine the association of 24-hour ABPM patterns with in-office orthostatic systolic BP (SBP) changes, extremely low standing and high supine SBP, or orthostatic hypotension (OH).
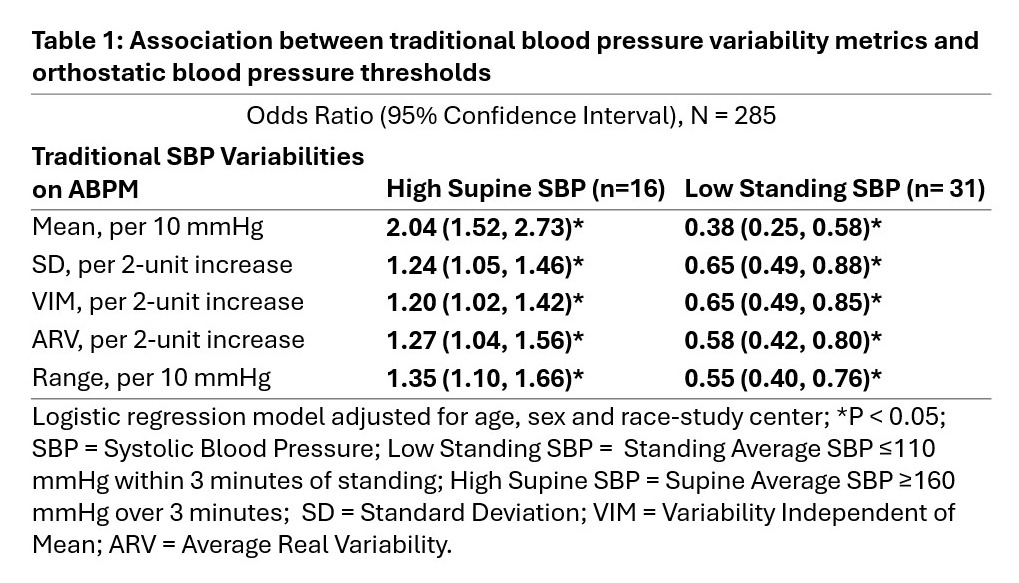
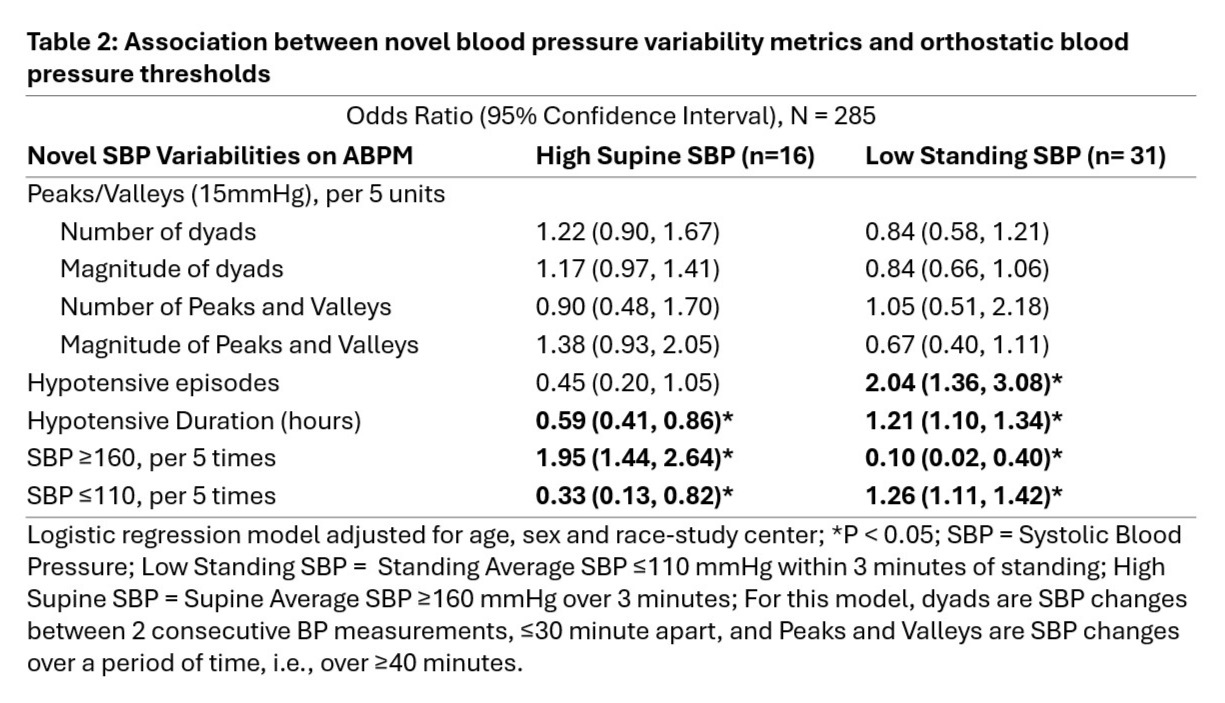
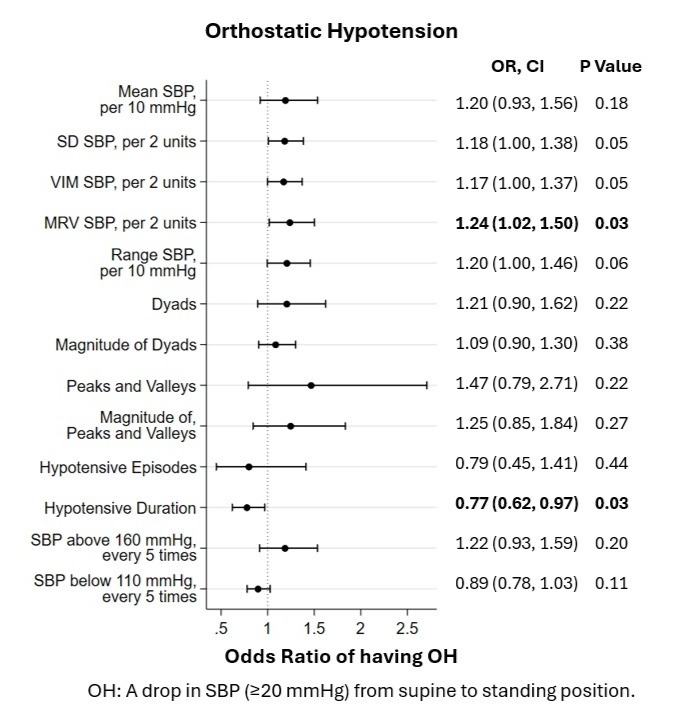
Methods: Participants in the Atherosclerosis Risk in Communities (ARIC) Study underwent ABPM and supine and standing in-clinic BP readings (2021-23). OH was defined (using a clinical BP device) as an average supine to standing drop in SBP (≥20 mmHg) (Figure). High average supine SBP (≥160 mmHg) and low average standing SBP (≤110 mmHg) were also measured. SBP variability using ABPM was defined with traditional metrics (Table 1), novel metrics (Table 2), SBP range on ABPM, and times SBP crossed high and low thresholds on ABPM. SBP dyads indicated short-term SBP changes, whereas peaks and valleys indicated gradual SBP changes. Hypotensive episodes and duration were also characterized. (Table 2) Associations of ABPM variability metrics with OH measures were determined via logistic regression adjusted for age, sex, and race-study center.
Results: Of the 285 participants with both ABPM and OH (44% male, mean age 83±3.5 years, mean SBP 129.3±12.8 mmHg), 15% (n=42) had OH. Higher SBP variability on ABPM was associated with low standing (OR = 0.38-0.65) and high supine SBP (OR = 1.20-2.04) (Table 1). Having low standing SBP was associated with a higher number of hypotensive episodes (OR = 2.04), hypotensive duration (OR = 1.21), ABPM SBP counts ≤110 mmHg (OR = 1.26), and inversely associated with ABPM SBP counts ≥160mmHg (OR = 0.10). Additionally, high supine SBP was associated with higher ABPM SBP counts ≥160mmHg (OR = 1.95) and inversely associated with hypotensive duration (OR = 0.59) and higher ABPM SBP counts ≤110 mmHg (OR = 0.33) (Table 2). Lastly, OH was associated with higher ARV (OR = 1.24) and inversely related to hypotensive duration (OR = 0.77) (Figure).
Conclusion: 24-hour ABPM variability metrics did not consistently associate with orthostatic SBP changes; however, they were associated with extremely low standing and high supine SBPs which relate to adverse outcomes in older adults. Future work should evaluate traditional and novel patterns on ABPM to characterize orthostatic changes and symptoms.
- Patil, Dhrumil ( BIDMC-Harvard Medical School , Boston , Massachusetts , United States )
- Cluett, Jennifer ( BIDMC-Harvard Medical School , Boston , Massachusetts , United States )
- Mukamal, Kenneth ( BETH ISRAEL DEACONESS MEDICAL CTR , Brookline , Massachusetts , United States )
- Coresh, Joe ( JOHNS HOPKINS SPH WELCH CENTER , Baltimore , Maryland , United States )
- Selvin, Elizabeth ( JOHNS HOPKINS UNIVERSITY , Baltimore , Maryland , United States )
- Wagenknecht, Lynne ( Wake Forest University School of Medicine , Winston Salem , North Carolina , United States )
- Hughes, Timothy ( Wake Forest University School of Medicine , Winston Salem , North Carolina , United States )
- Windham, B Gwen ( UMMC, The MIND Center , Jackson , Mississippi , United States )
- Mosley, Thomas ( UNIV MS MEDICAL CTR , Jackson , Mississippi , United States )
- Lutsey, Pamela ( University of Minnesota , Minneapolis , Minnesota , United States )
- Ring, Kimberly ( UNC - Biostatistics , Chapel Hill , North Carolina , United States )
- Xue, Catherine ( Harvard University , Boston , Massachusetts , United States )
- Lipsitz, Lewis ( Harvard University , Boston , Massachusetts , United States )
- Ma, Yuan ( Harvard University , Boston , Massachusetts , United States )
- Valint, Arielle ( UNC- Chapel Hill , Chapel Hill , North Carolina , United States )
- Juraschek, Stephen ( BIDMC-Harvard Medical School , Boston , Massachusetts , United States )
- Khan, Md Marufuzzaman ( Beth Israel Deaconess Medical Cente , Brookline , Massachusetts , United States )
- Col, Hannah ( Beth Israel Deaconess Medical Center , Boston , Massachusetts , United States )
- Larbi, Fredrick ( Beth Israel Deaconess Medical Ctr , Boston , Massachusetts , United States )
- Zhang, Wenxin ( Harvard University , Boston , Massachusetts , United States )
- Zhang, Mingyu ( Harvard Medical School , Boston , Massachusetts , United States )
- Turkson-ocran, Ruth-alma ( Beth Israel Deaconess Medical Ctr , Boston , Massachusetts , United States )
- Ngo, Long ( Harvard Medical School , Boston , Massachusetts , United States )
Meeting Info:
Session Info:
Poster Session 1 and Reception (includes TAC Poster Competition)
Thursday, 09/04/2025 , 05:30PM - 07:00PM
Poster Session
More abstracts on this topic:
Weber Michael, Bakris George, Flack John, Gimona Alberto, Narkiewicz Krzysztof, Sassi-sayadi Mouna, Wang Jiguang, Schlaich Markus
A pilot study of an intervention for self-management of blood pressure among refugees fleeing war and resettled in the United StatesBehnam Rawnaq, Godino Job, Celis Deisy, Anderson Cheryl, Al-rousan Tala
More abstracts from these authors:
Khan Md Marufuzzaman, Coresh Joe, Selvin Elizabeth, Wagenknecht Lynne, Hughes Timothy, Windham B Gwen, Mosley Thomas, Lutsey Pamela, Ring Kimberly, Lipsitz Lewis, Valint Arielle, Col Hannah, Juraschek Stephen, Larbi Fredrick, Patil Dhrumil, Zhang Mingyu, Turkson-ocran Ruth-alma, Ngo Long, Cluett Jennifer, Mukamal Kenneth
Frailty and Sex are associated with Discordant Blood Pressure Measures among Very Old Adults: Results from the Atherosclerosis Risk in Communities (ARIC) StudyLarbi Fredrick, Coresh Joe, Selvin Elizabeth, Wagenknecht Lynne, Hughes Timothy, Windham B Gwen, Mosley Thomas, Lutsey Pamela, Ring Kimberly, Juraschek Stephen, Khan Md Marufuzzaman, Col Hannah, Patil Dhrumil, Zhang Mingyu, Turkson-ocran Ruth-alma, Ngo Long, Cluett Jennifer, Mukamal Kenneth