Final ID: MP-20
Leveraging Electronic Health Records to Assess Neighborhood Advantages and Risk of Cardiovascular Outcomes Among Hypertensive Patients
Abstract Body: Introduction: Hypertension disproportionately impacts socially disadvantaged groups in the U.S. with increasing prevalence and suboptimal control rates. Our study aims to examine the association between neighborhood-level social vulnerability and hypertension outcomes using electronic health record (EHR) data from a large regional health system.
Methods: We conducted a retrospective analysis of EHR data from the Sentara Health System, covering the period from January 1st, 2010, to December 31st, 2022. We assigned a Social Vulnerability Index (SVI) based on the residential census tract of each patient and established a longitudinal cohort of patients who consistently utilized healthcare services. To be included in the study, patients were required to have a minimum of five years of observational time and to have healthcare visits in at least 50% of the observed years. The study focused on patients diagnosed with hypertension—either through a hypertension diagnosis, a blood pressure measurement exceeding 140/90, or antihypertensive medication prescriptions. We utilized multivariate Cox Proportional Hazards models to analyze the associations of SVI with cardiovascular outcomes and blood pressure control (<140/90 mmHg).
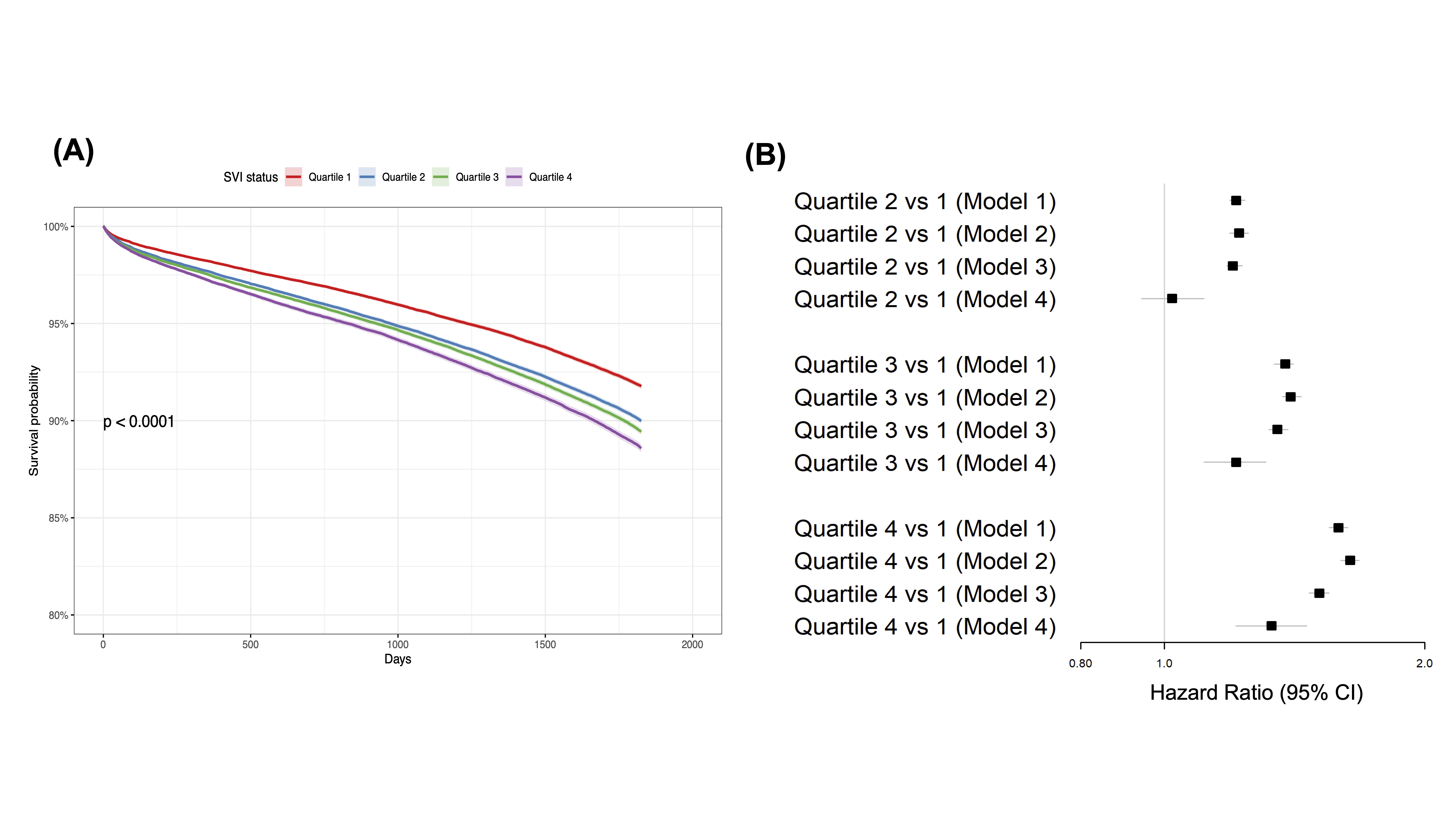
Results: The longitudinal cohort consisted of 55,060 patients, with an average age of 54 years (Interquartile range: 42-65), 30.0% of whom were Black adults and 60.0% were females. Compared to patients residing in the most advantaged neighborhoods (quartile 1 of SVI), those in more disadvantaged neighborhoods (quartiles 2, 3, and 4) had hazard ratios for composite cardiovascular endpoint (myocardial infarction, heart failure, and stroke) of 1.22 (95% CI, 1.19-1.25), 1.40 (95% CI, 1.37-1.44), and 1.64 (95% CI, 1.60-1.68), respectively, after adjustment for age and sex. Additionally, blood pressure control was significantly lower in higher SVI quartiles, with control rates in quartiles 1 through 4 at 78.4%, 76.5%, 75.2%, and 72.8%, respectively (P<0.001). Among the SVI themes, socioeconomic status (theme 1) and housing type and transportation (theme 4) were associated with the highest hazard ratios for cardiovascular outcomes.
Conclusions: Neighborhood-level social vulnerability is significantly associated with worse hypertension control and adverse cardiovascular outcomes. Health systems can employ tailored interventions targeting high-risk neighborhoods to reduce disparities and enhance health outcomes for vulnerable populations.
Methods: We conducted a retrospective analysis of EHR data from the Sentara Health System, covering the period from January 1st, 2010, to December 31st, 2022. We assigned a Social Vulnerability Index (SVI) based on the residential census tract of each patient and established a longitudinal cohort of patients who consistently utilized healthcare services. To be included in the study, patients were required to have a minimum of five years of observational time and to have healthcare visits in at least 50% of the observed years. The study focused on patients diagnosed with hypertension—either through a hypertension diagnosis, a blood pressure measurement exceeding 140/90, or antihypertensive medication prescriptions. We utilized multivariate Cox Proportional Hazards models to analyze the associations of SVI with cardiovascular outcomes and blood pressure control (<140/90 mmHg).
Results: The longitudinal cohort consisted of 55,060 patients, with an average age of 54 years (Interquartile range: 42-65), 30.0% of whom were Black adults and 60.0% were females. Compared to patients residing in the most advantaged neighborhoods (quartile 1 of SVI), those in more disadvantaged neighborhoods (quartiles 2, 3, and 4) had hazard ratios for composite cardiovascular endpoint (myocardial infarction, heart failure, and stroke) of 1.22 (95% CI, 1.19-1.25), 1.40 (95% CI, 1.37-1.44), and 1.64 (95% CI, 1.60-1.68), respectively, after adjustment for age and sex. Additionally, blood pressure control was significantly lower in higher SVI quartiles, with control rates in quartiles 1 through 4 at 78.4%, 76.5%, 75.2%, and 72.8%, respectively (P<0.001). Among the SVI themes, socioeconomic status (theme 1) and housing type and transportation (theme 4) were associated with the highest hazard ratios for cardiovascular outcomes.
Conclusions: Neighborhood-level social vulnerability is significantly associated with worse hypertension control and adverse cardiovascular outcomes. Health systems can employ tailored interventions targeting high-risk neighborhoods to reduce disparities and enhance health outcomes for vulnerable populations.
More abstracts on this topic:
A Key Role of Proximal Tubule Renin-Angiotensin System in The Kidney in The Development of Kidney Ischemia and Reperfusion Injury
Li Xiao, Hassan Rumana, Katsurada Akemi, Sato Ryosuke, Zhuo Jia
A Focus for Improvement - Factors for Lab Adherence in a Pediatric Preventive Cardiology ProgramHolsinger Hunter, Porterfield Ronna, Taylor Makenna, Dresbach Bethany, Seipel Brittany, Igwe Chukwuemeka, Alvarado Chance, Tran Andrew