Final ID: P-105
Comparative Effectiveness between Angiotensin Receptor Blockers and Angiotensin-Converting Enzyme Inhibitors on Mortality: a Nationwide, Population-based, Prospective Cohort Study in China
Abstract Body: Background: Contemporary evidence comparing the efficacy of angiotensin-converting enzyme inhibitors (ACEIs) versus angiotensin II receptor blockers (ARBs) on long-term outcomes in patients with hypertension is sparse and inconsistent. The aim is to compare the effectiveness of ACEI monotherapy versus ARB monotherapy on all-cause death and cardiovascular death.
Methods: Based on a nationwide, population-based prospective cohort project, which covered 318 study sites from 2014 to 2021 in China. Detailed information was collected by questionnaire, physical measurement, and blood test. Participants aged 35-75 years with hypertension and taking ACEI or ARB monotherapy once daily, and with good medication adherence at baseline were included. Information on mortality was followed up until 31 December 2021. Stabilized inverse probability treatment weighting (IPTW) was applied to compare the effectiveness.
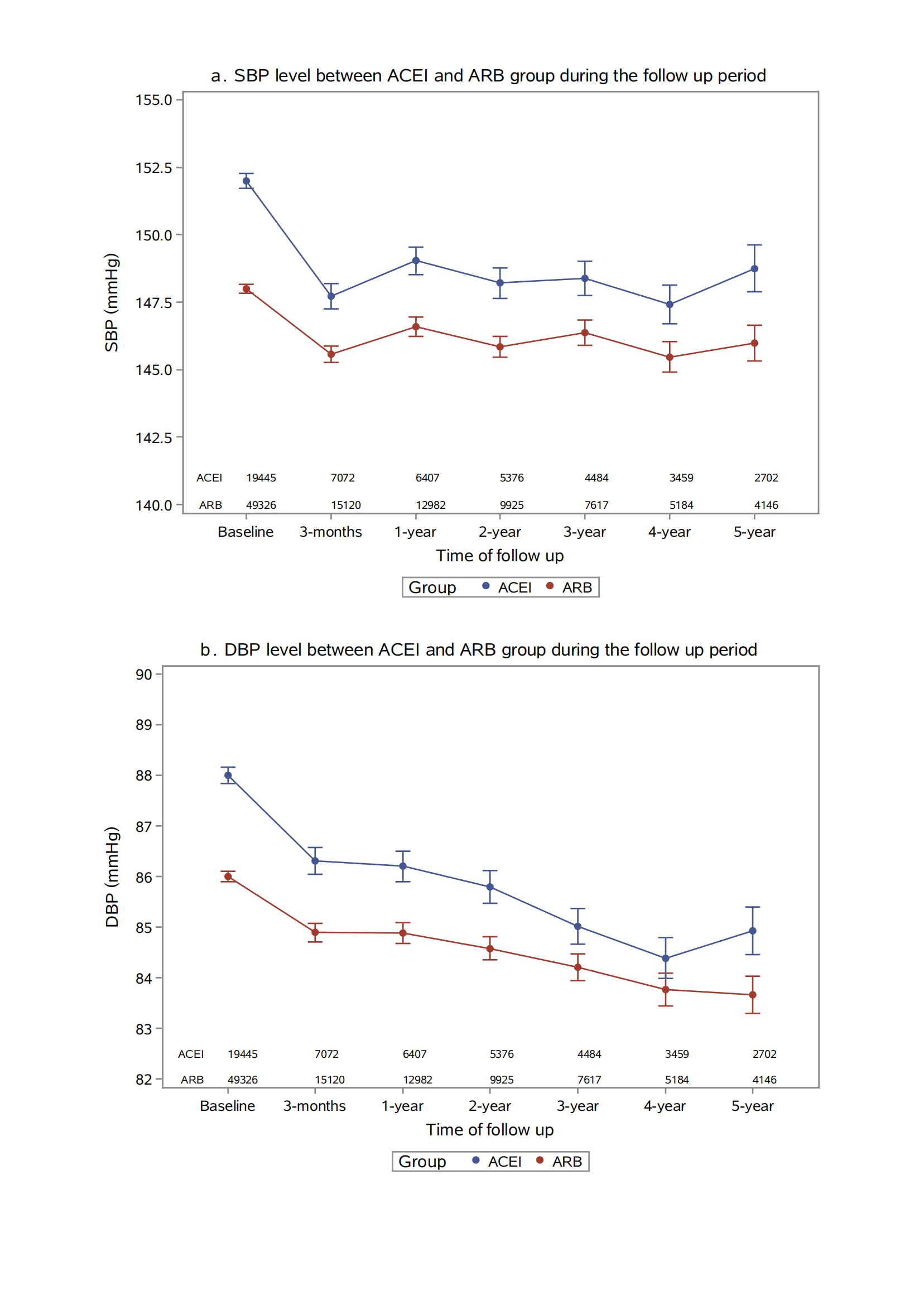
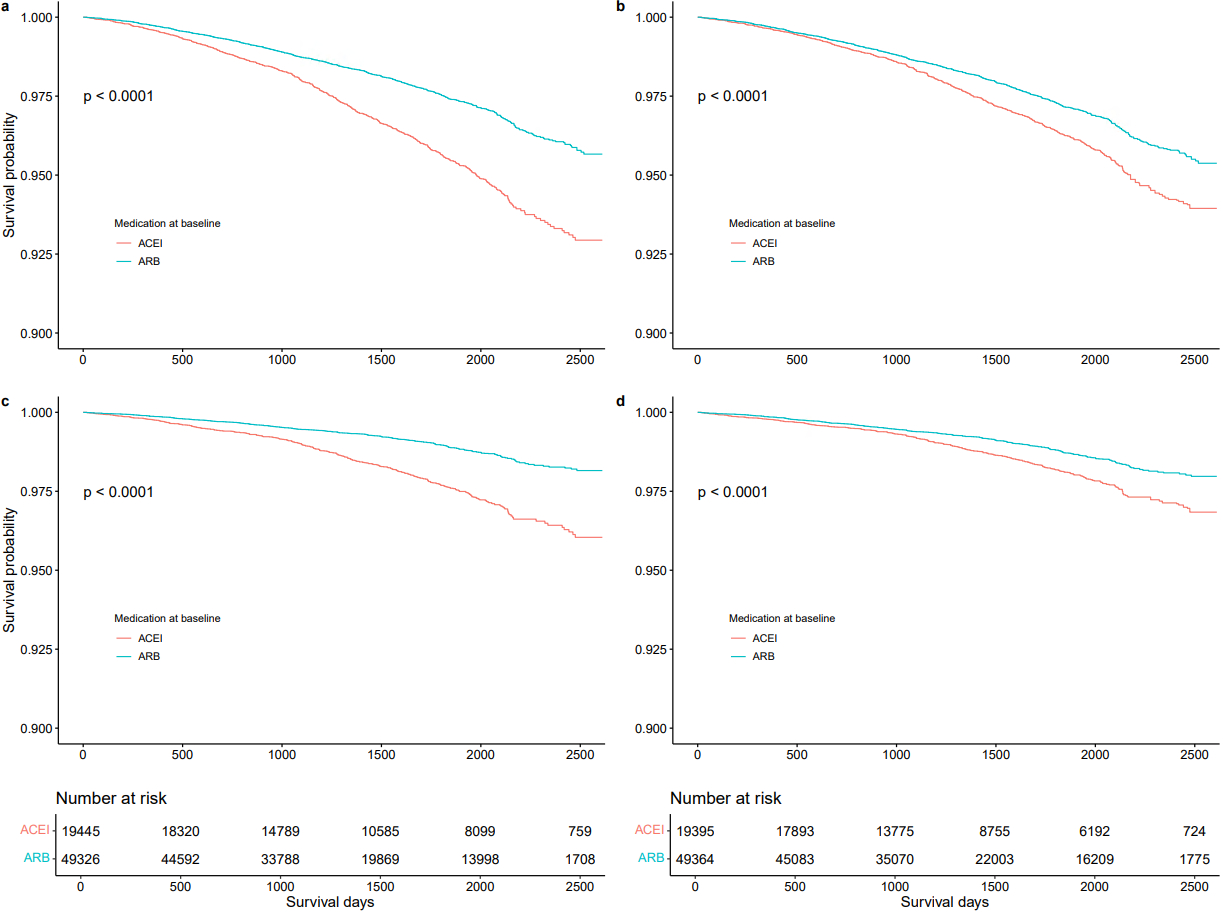
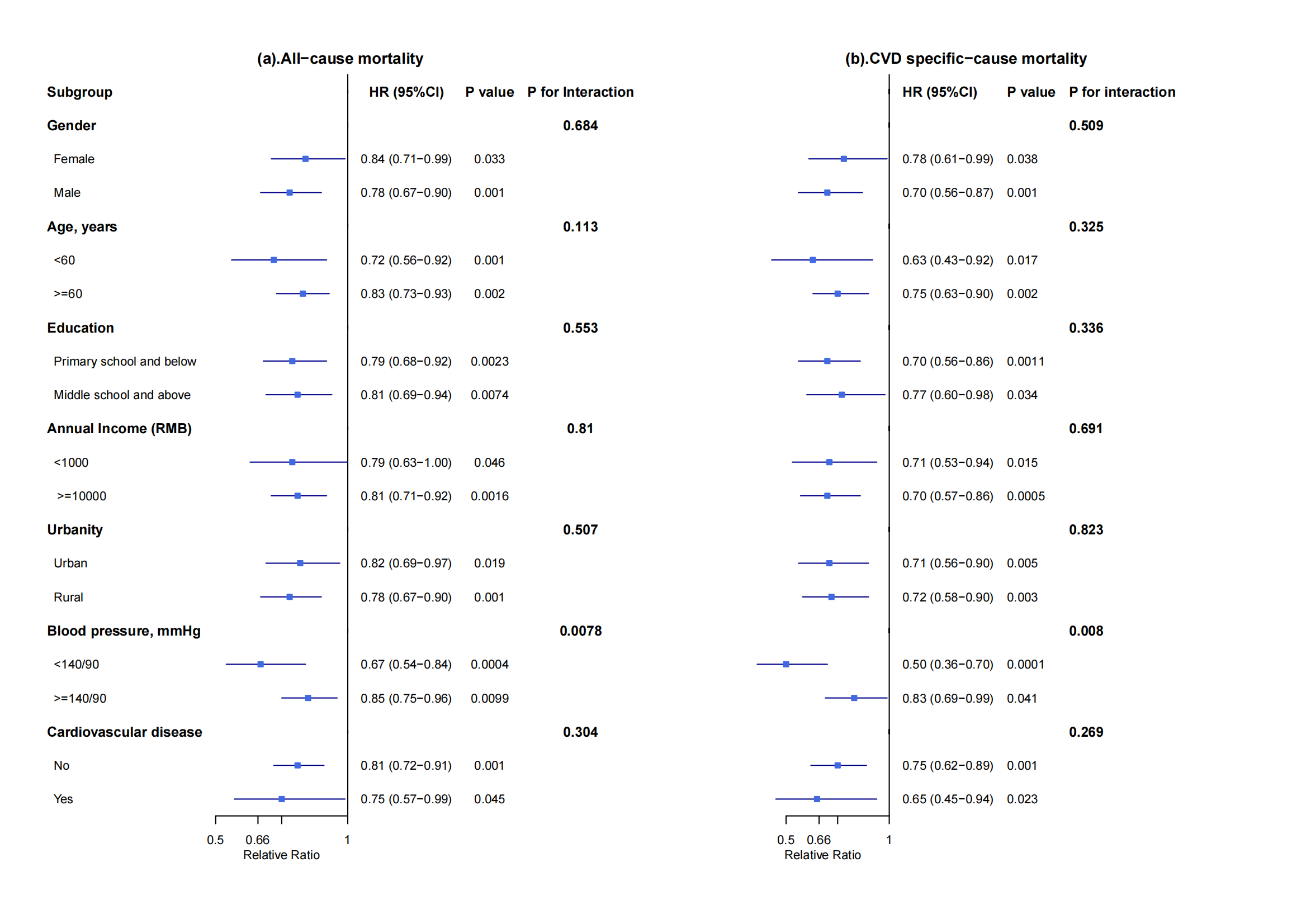
Results: 68 771 (49326 ARB, 19445 ACEI) participants were finally included, with a mean age of 59.9±8.3 years and 40.2% being female. During a median follow-up time of 44 months, 785 cardiovascular deaths and 1657 deaths were recorded. Compared with ACEI monotherapy, ARB monotherapy was associated with a quarter relative risk reduction of cardiovascular death (IPTW rates: 0.95 % Vs 1.43%, HR=0.73 [95%CI, 0.62-0.87]) and one-fifth relative risk reduction of all-cause death (IPTW rates: 2.13% Vs 2.84%, HR=0.80 [95%CI, 0.71-0.89]). These differences remained consistent after further adjusting for blood pressure and with differences more pronounced in patients with controlled and newly onset hypertension. Sensitive analysis and subgroup analysis yielded consistent results.
Conclusions: Attention should be paid that ARB can be preferred to ACEI in patients with hypertension in terms of long-term health outcomes.
Funding: This work was supported by the Chinese Academy of Medical Sciences Innovation Fund for Medical Science (2021-I2M-1-011), and the National High Level Hospital Clinical Research Funding (2022-GSP-GG-4, NCRCSZ-2023-016).
Keywords: Hypertension, Angiotensin receptor blocker, Angiotensin-converting enzyme inhibitor, Mortality, Comparative effectiveness
Methods: Based on a nationwide, population-based prospective cohort project, which covered 318 study sites from 2014 to 2021 in China. Detailed information was collected by questionnaire, physical measurement, and blood test. Participants aged 35-75 years with hypertension and taking ACEI or ARB monotherapy once daily, and with good medication adherence at baseline were included. Information on mortality was followed up until 31 December 2021. Stabilized inverse probability treatment weighting (IPTW) was applied to compare the effectiveness.
Results: 68 771 (49326 ARB, 19445 ACEI) participants were finally included, with a mean age of 59.9±8.3 years and 40.2% being female. During a median follow-up time of 44 months, 785 cardiovascular deaths and 1657 deaths were recorded. Compared with ACEI monotherapy, ARB monotherapy was associated with a quarter relative risk reduction of cardiovascular death (IPTW rates: 0.95 % Vs 1.43%, HR=0.73 [95%CI, 0.62-0.87]) and one-fifth relative risk reduction of all-cause death (IPTW rates: 2.13% Vs 2.84%, HR=0.80 [95%CI, 0.71-0.89]). These differences remained consistent after further adjusting for blood pressure and with differences more pronounced in patients with controlled and newly onset hypertension. Sensitive analysis and subgroup analysis yielded consistent results.
Conclusions: Attention should be paid that ARB can be preferred to ACEI in patients with hypertension in terms of long-term health outcomes.
Funding: This work was supported by the Chinese Academy of Medical Sciences Innovation Fund for Medical Science (2021-I2M-1-011), and the National High Level Hospital Clinical Research Funding (2022-GSP-GG-4, NCRCSZ-2023-016).
Keywords: Hypertension, Angiotensin receptor blocker, Angiotensin-converting enzyme inhibitor, Mortality, Comparative effectiveness
More abstracts on this topic:
A cerebrovascular longitudinal atlas: different rates of morphological change in aneurysm patients associated with hypertension and diabetes
A Longitudinal 20-year Analysis Indicates Acceleration of Cardiometabolic Comorbidities on Dementia Risk
Chien Aichi, Salamon Noriko, Vinuela Fernando, Szeder Viktor, Colby Geoffrey, Jahan Reza, Boyle Noel, Villablanca Juan, Duckwiler Gary
A Longitudinal 20-year Analysis Indicates Acceleration of Cardiometabolic Comorbidities on Dementia Risk
Lihua Huang, Danish Muhammad, Auyeung Tw, Jenny Lee, Kwok Timothy, Abrigo Jill, Wei Yingying, Lo Cecilia, Fung Erik