Final ID: P-176
Elevated Circulating T Cell-Monocyte Complexes in Long COVID-19 Tachycardia Syndrome: Implications of Immune Dysregulation, Inflammation, and Disease Progression
Abstract Body: BACKGROUND: Postural orthostatic tachycardia syndrome (POTS) is a common complication in Long-COVID. Long-COVID POTS (LCP) is characterized by abnormal orthostatic tachycardia, symptoms of orthostatic intolerance, and persistent inflammation.
HYPOTHESIS: Novel parameters of immune activation exist in and likely contribute to the pathogenesis of LCP.
METHODS: We enrolled 15 LCP patients and 5 subjects who recovered from COVID-19 infection without lingering effects as controls. Hemodynamic parameters were measured at baseline and during a 10-minute 75° head-up tilt. Flow cytometry was used to detect circulating T cells, monocyte subsets, and their cytokines. Immune synapse formation between T cells and monocytes was detected using Forster Resonance Energy Transfer (FRET) between T cell receptors (TCR) and human leukocyte antigens (HLAs). Intracellular staining was used to detect the cytokines IL-17A, IFN-γ and IL-6.
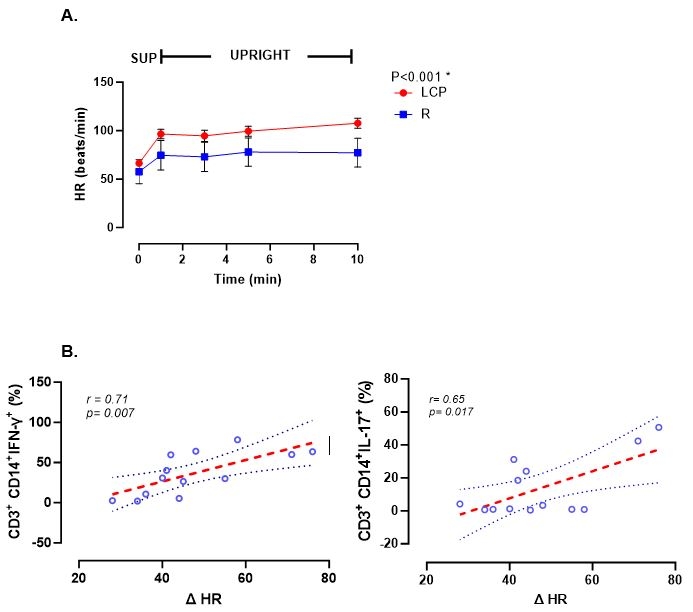
RESULTS: Subjects with LCP exhibited a greater increase in heart rate (HR) during 10-min upright tilt compared with controls (50.23± 4.6 vs. 20.33 ± 3.17 bpm, p<0.01, Figure). Circulating monocyte/T cell complexes were increased in LCP vs controls and these exhibited high TCR/HLA FRET (p<0.005), suggesting immune synapse formation. Importantly, complexed T cells demonstrated higher levels of IL-17A and IFN-γ, compared to non-complexed T cells and a profound increase in intracellular IL-6 compared to non-complexed monocytes (p<0.005). Notably, the percent of IFN-γ+ and IL-17A+ T cells in the monocyte/T cell complexes of LCP subjects positively correlated with their increase in HR (ΔHR) in 10 min active standing test (Figure).
CONCLUSION: Circulating T cell-monocyte complexes are markedly increased in humans with LPC, and exhibit evidence of functional and dynamic cellular interactions. We propose that these contribute to persistent inflammation and the pathogenesis of autonomic dysfunction in these subjects.
HYPOTHESIS: Novel parameters of immune activation exist in and likely contribute to the pathogenesis of LCP.
METHODS: We enrolled 15 LCP patients and 5 subjects who recovered from COVID-19 infection without lingering effects as controls. Hemodynamic parameters were measured at baseline and during a 10-minute 75° head-up tilt. Flow cytometry was used to detect circulating T cells, monocyte subsets, and their cytokines. Immune synapse formation between T cells and monocytes was detected using Forster Resonance Energy Transfer (FRET) between T cell receptors (TCR) and human leukocyte antigens (HLAs). Intracellular staining was used to detect the cytokines IL-17A, IFN-γ and IL-6.
RESULTS: Subjects with LCP exhibited a greater increase in heart rate (HR) during 10-min upright tilt compared with controls (50.23± 4.6 vs. 20.33 ± 3.17 bpm, p<0.01, Figure). Circulating monocyte/T cell complexes were increased in LCP vs controls and these exhibited high TCR/HLA FRET (p<0.005), suggesting immune synapse formation. Importantly, complexed T cells demonstrated higher levels of IL-17A and IFN-γ, compared to non-complexed T cells and a profound increase in intracellular IL-6 compared to non-complexed monocytes (p<0.005). Notably, the percent of IFN-γ+ and IL-17A+ T cells in the monocyte/T cell complexes of LCP subjects positively correlated with their increase in HR (ΔHR) in 10 min active standing test (Figure).
CONCLUSION: Circulating T cell-monocyte complexes are markedly increased in humans with LPC, and exhibit evidence of functional and dynamic cellular interactions. We propose that these contribute to persistent inflammation and the pathogenesis of autonomic dysfunction in these subjects.
More abstracts on this topic:
A Non-invasive In Vivo Experimental Model of Heart Failure Using Optogenetic Tachypacing in Larval Zebrafish
Savoie Emma, Ramadan Ahmed, Purvis Katherine, Stoyek Matthew, Quinn Alex
A Novel Role for Lipoprotein(a) in Potentiating Neutrophil Extracellular Trap FormationMouawad Sahar, Boffa Michael, Koschinsky Marlys