Final ID: P3174
The Benefits of Probiotic Administration in Stroke Risk, Stroke-Related Gastrointestinal Complications, and Intestinal Flora Dysbiosis: A Meta-Meta-Analysis
Abstract Body:
INTRODUCTION
Stroke is the second largest cause of death and third leading cause of disability worldwide. Some high-income countries have one in five lifetime cases and one in two in low-income countries. Due to the high stroke burden and aging population, better preventive and treatment approaches are needed. Recent research shows that stroke patients have a different gut microbiota than healthy people, suggesting a relationship between dysbiosis and stroke incidence and prognosis. Probiotics may improve stroke outcomes by strengthening the intestinal barrier and reducing inflammation.
HYPOTHESIS
Our study seeks to evaluate the potential benefits of probiotic supplementation in reducing the risk of ischemic stroke in healthy individuals as well as its impact on the prognosis of stroke patients, specifically in reducing gastrointestinal complications and improving gut microbiota balance (reduce dysbiosis).
METHODS
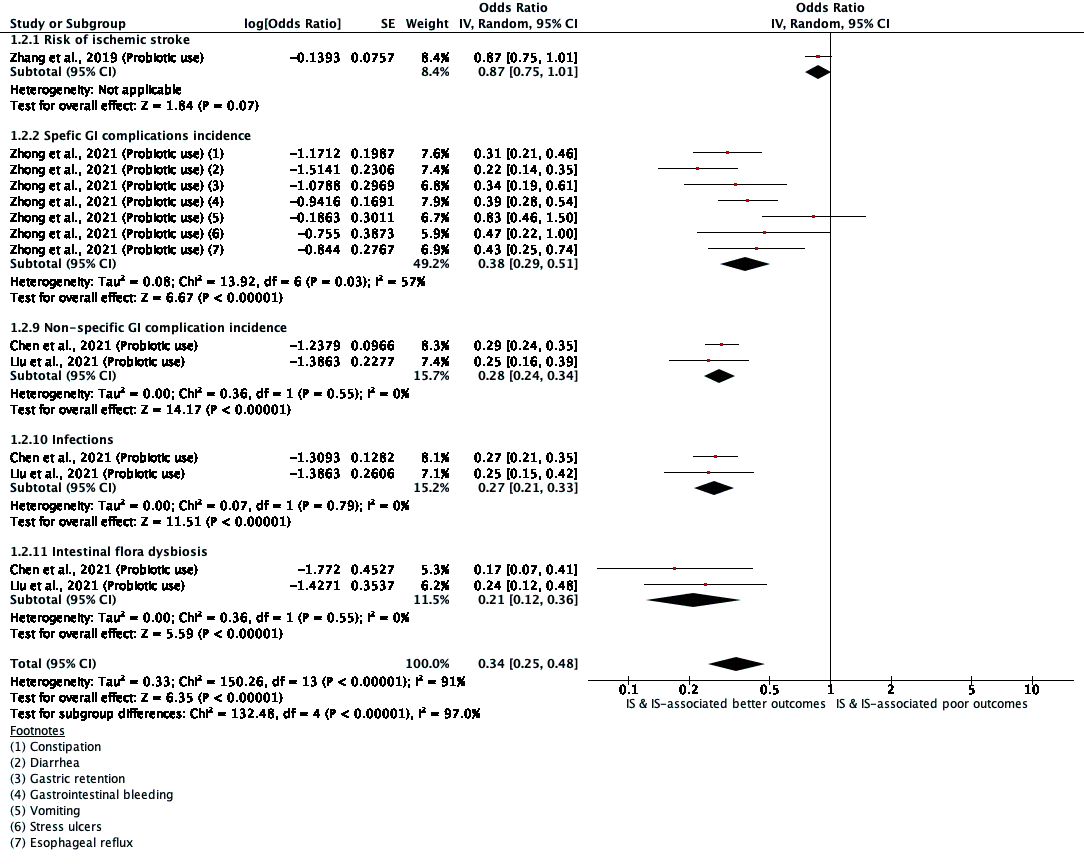
We conducted an umbrella meta-analysis of meta-analyses published in the last 10 years using PRISMA guidelines in PubMed. Using RevMan 5.4, we performed an inverse variance random effects model to calculate log (odds ratio) and converted it to pooled OR and 95% confidence interval to obtain a forest plot keeping alpha criteria 0.05. Heterogeneity and risk of bias assessment (by Newcastle-Ottawa Scale) were assessed.
RESULTS
While probiotic supplementation in healthy individuals did not significantly decrease the risk of ischemic stroke (OR 0.87 [95%CI 0.75-1.01]), it showed notable benefits in stroke patients. These positive effects included a substantial reduction in the odds of specific GI complications (constipation, diarrhea, gastric retention, esophageal reflux, vomiting, stress ulcers, and gastrointestinal bleeding) by 62% (0.38, 0.29-0.51), non-specific GI complications by 72% (0.28, 0.24-0.34), infection by 73% (0.27, 0.21-0.33) and a significant improvement in gut flora balance, reducing the odds of dysbiosis by 79% (0.21, 0.12-0.36). (p<0.00001) The inter-study heterogeneity was 91% with (p<0.00001, Chi2=128.76), a moderate risk of bias.
CONCLUSION
Our umbrella meta-analysis highlights the potential benefits of probiotic supplementation in stroke patients, particularly in mitigating stroke-related GI complications and alleviating intestinal flora dysbiosis. These findings underscore the crucial role of gut-brain interactions in stroke and suggest that probiotics may serve as a promising component of stroke management.
INTRODUCTION
Stroke is the second largest cause of death and third leading cause of disability worldwide. Some high-income countries have one in five lifetime cases and one in two in low-income countries. Due to the high stroke burden and aging population, better preventive and treatment approaches are needed. Recent research shows that stroke patients have a different gut microbiota than healthy people, suggesting a relationship between dysbiosis and stroke incidence and prognosis. Probiotics may improve stroke outcomes by strengthening the intestinal barrier and reducing inflammation.
HYPOTHESIS
Our study seeks to evaluate the potential benefits of probiotic supplementation in reducing the risk of ischemic stroke in healthy individuals as well as its impact on the prognosis of stroke patients, specifically in reducing gastrointestinal complications and improving gut microbiota balance (reduce dysbiosis).
METHODS
We conducted an umbrella meta-analysis of meta-analyses published in the last 10 years using PRISMA guidelines in PubMed. Using RevMan 5.4, we performed an inverse variance random effects model to calculate log (odds ratio) and converted it to pooled OR and 95% confidence interval to obtain a forest plot keeping alpha criteria 0.05. Heterogeneity and risk of bias assessment (by Newcastle-Ottawa Scale) were assessed.
RESULTS
While probiotic supplementation in healthy individuals did not significantly decrease the risk of ischemic stroke (OR 0.87 [95%CI 0.75-1.01]), it showed notable benefits in stroke patients. These positive effects included a substantial reduction in the odds of specific GI complications (constipation, diarrhea, gastric retention, esophageal reflux, vomiting, stress ulcers, and gastrointestinal bleeding) by 62% (0.38, 0.29-0.51), non-specific GI complications by 72% (0.28, 0.24-0.34), infection by 73% (0.27, 0.21-0.33) and a significant improvement in gut flora balance, reducing the odds of dysbiosis by 79% (0.21, 0.12-0.36). (p<0.00001) The inter-study heterogeneity was 91% with (p<0.00001, Chi2=128.76), a moderate risk of bias.
CONCLUSION
Our umbrella meta-analysis highlights the potential benefits of probiotic supplementation in stroke patients, particularly in mitigating stroke-related GI complications and alleviating intestinal flora dysbiosis. These findings underscore the crucial role of gut-brain interactions in stroke and suggest that probiotics may serve as a promising component of stroke management.
More abstracts on this topic:
Beyond the Cuff: Revolutionizing Hypertension Care through Human-Centered Design and Tech-Driven Solutions in an Urban Community Health Center
Khan Aisha, Mcauliff Kathleen, Govindarajan Geetha
Aberrant MicroRNA Expression May Underlie Cardiac Dysfunction in a rat model of PreeclampsiaVaka Ramana, Campbell Nathan, Edwards Kristin, Hoang Ngoc, Zheng Baoying, Lamarca Babbette