Final ID: MP11
Short-Term Dual Antiplatelet Therapy Following Percutaneous Intervention Does Not Impact Stroke Outcomes: A Meta-Analysis of Randomized Controlled Trials
Abstract Body (Do not enter title and authors here): Background
Dual-antiplatelet therapy (DAPT) is recommended after percutaneous coronary intervention (PCI) to reduce recurrent ischemic events, though optimal duration is unclear. Current U.S. and European guidelines recommend 6-month and 12-month durations of DAPT following PCI for stable coronary disease, and acute coronary syndrome (ACS), respectively. Recent randomized controlled trials (RCTs) have suggested that shorter durations of DAPT following PCI may result in similar ischemic outcomes, while decreasing risk of major bleeding events. The impact of shorter DAPT durations on ischemic and hemorrhagic cerebrovascular events remains unclear.
Hypothesis
Shorter duration of DAPT therapy is associated with decreased hemorrhagic stroke risk and similar ischemic stroke risk, as compared to traditional DAPT regimens.
Methods
PubMed, EMBASE, and Cochrane databases were queried from inception to June 2025 to identify RCTs comparing short-term (≤3 months) with traditional durations of DAPT following PCI. Outcomes of interest include ischemic stroke, hemorrhagic stroke, and total cerebrovascular events. Effect estimates were pooled with random effects models and reported as risk ratios for dichotomous outcomes and mean differences for continuous variables using 95% confidence intervals.
Results
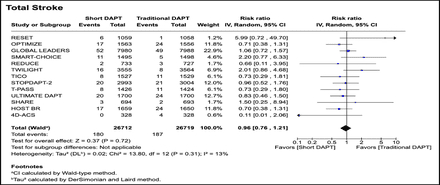
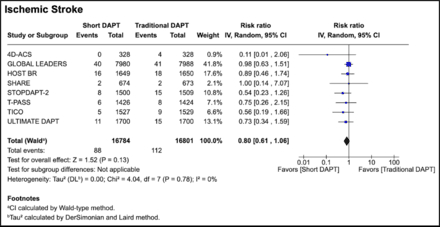
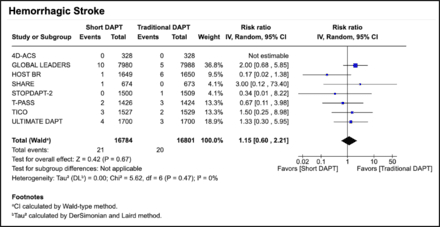
Thirteen studies met inclusion criteria comprising 53,421 patients (mean age 64 years; 76% male, 64% presenting with ACS). All reported all-cause strokes; only seven studies reported stroke subtypes. Of these seven, four studies followed short DAPT with ticagrelor monotherapy, two used clopidogrel, and one used prasugrel. Two studies used a duration of three months for the short DAPT arm, while the other five studies used a duration of ≤1 month. Shorter duration of DAPT resulted in no significant difference in rates of total stroke (RR: 0.96; [0.76, 1.21] p=0.31). Interestingly, the incidence of ischemic stroke was lower in the short DAPT cohort, although this did not reach statistical significance (RR: 0.80; [0.61, 1.06] p=0.13). The incidence of hemorrhagic stroke was higher in the short DAPT group, though this also was not statistically significant (RR: 1.15; [0.60, 2.21] p=0.67).
Conclusions
While there were no differences in overall stroke rates between the short and traditional DAPT cohorts, there is a trend toward lower incidence of ischemic stroke and higher incidence of hemorrhagic stroke in patients receiving short DAPT compared to traditional DAPT regimens.
Dual-antiplatelet therapy (DAPT) is recommended after percutaneous coronary intervention (PCI) to reduce recurrent ischemic events, though optimal duration is unclear. Current U.S. and European guidelines recommend 6-month and 12-month durations of DAPT following PCI for stable coronary disease, and acute coronary syndrome (ACS), respectively. Recent randomized controlled trials (RCTs) have suggested that shorter durations of DAPT following PCI may result in similar ischemic outcomes, while decreasing risk of major bleeding events. The impact of shorter DAPT durations on ischemic and hemorrhagic cerebrovascular events remains unclear.
Hypothesis
Shorter duration of DAPT therapy is associated with decreased hemorrhagic stroke risk and similar ischemic stroke risk, as compared to traditional DAPT regimens.
Methods
PubMed, EMBASE, and Cochrane databases were queried from inception to June 2025 to identify RCTs comparing short-term (≤3 months) with traditional durations of DAPT following PCI. Outcomes of interest include ischemic stroke, hemorrhagic stroke, and total cerebrovascular events. Effect estimates were pooled with random effects models and reported as risk ratios for dichotomous outcomes and mean differences for continuous variables using 95% confidence intervals.
Results
Thirteen studies met inclusion criteria comprising 53,421 patients (mean age 64 years; 76% male, 64% presenting with ACS). All reported all-cause strokes; only seven studies reported stroke subtypes. Of these seven, four studies followed short DAPT with ticagrelor monotherapy, two used clopidogrel, and one used prasugrel. Two studies used a duration of three months for the short DAPT arm, while the other five studies used a duration of ≤1 month. Shorter duration of DAPT resulted in no significant difference in rates of total stroke (RR: 0.96; [0.76, 1.21] p=0.31). Interestingly, the incidence of ischemic stroke was lower in the short DAPT cohort, although this did not reach statistical significance (RR: 0.80; [0.61, 1.06] p=0.13). The incidence of hemorrhagic stroke was higher in the short DAPT group, though this also was not statistically significant (RR: 1.15; [0.60, 2.21] p=0.67).
Conclusions
While there were no differences in overall stroke rates between the short and traditional DAPT cohorts, there is a trend toward lower incidence of ischemic stroke and higher incidence of hemorrhagic stroke in patients receiving short DAPT compared to traditional DAPT regimens.
More abstracts on this topic:
An Unusual Presentation of Cerebellar Stroke Following the Removal of Microaxial Flow Pump
Liu Zi Qian, Alsheikh-kassim Mohammad, Karpenos Joseph, Frodey Kevin
Anticoagulation versus Antiplatelets Across Subgroups of Embolic Stroke of Undetermined Source: A Meta-Analysis of Seven Randomized Controlled TrialsGhannam Malik, Elkind Mitchell, Tirschwell David, Poli Sven, Kamel Hooman, Yaghi Shadi, Al-qudah Abdullah, Alshaer Qasem, Kronmal Richard, Ntaios George, Longstreth W, Furie Karen, Saver Jeffrey, Kasner Scott