Final ID: Su3024
Demographic Inequities in Catheter Ablation Among SVT Hospitalizations: An Analysis of the Nationwide Inpatient Sample Database
Abstract Body (Do not enter title and authors here): Background:
Catheter ablation is a guideline-directed therapy for symptomatic supraventricular tachycardia (SVT), yet disparities in its utilization across patient populations remain inadequately characterized.
Objective:
To evaluate demographic and hospital-level factors associated with catheter ablation among hospitalized patients with SVT in the United States.
Methods:
We analyzed adult hospitalizations with a diagnosis of SVT (ICD-10-CM I47.1) from the National Inpatient Sample (NIS) for the years 2016 through 2020. Catheter ablation was identified using ICD-10-PCS procedure codes. Survey-weighted logistic regression was used to assess associations between demographic characteristics and the odds of receiving ablation. Age was evaluated both as a continuous and categorical variable. Analyses accounted for the complex survey design of the NIS.
Results:
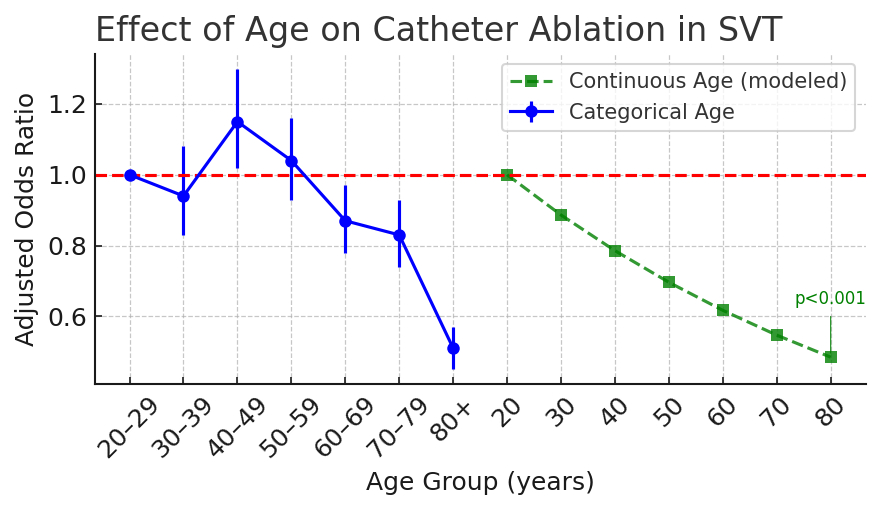
Among approximately 1.87 million weighted hospitalizations for SVT, only 4.1% underwent catheter ablation. Female patients comprised 52.5% of the SVT cohort but had 16.0% lower odds of receiving ablation compared to males (adjusted OR [aOR] 0.84; p<0.001). Black patients had 9.1% lower odds of ablation compared to White patients (aOR 0.91; p=0.002), while Hispanic and Other race groups had 18.1% (aOR 1.18; p<0.001) and 24.6% (aOR 1.25; p=0.003) higher odds, respectively. Insurance status also impacted access: patients with private insurance had 34.2% higher odds of ablation compared to Medicare recipients (aOR 1.34; p<0.001), whereas those with Medicaid had 9.7% lower odds (aOR 0.90; p=0.010). Increasing age was inversely associated with ablation use, with a 1.2% decrease in odds per year of age (aOR 0.99; 95% CI 0.987–0.989; p<0.001). Compared to patients aged 20–29, those aged 40–49 had 15.4% higher odds (aOR 1.15; p=0.018), while patients aged 60–69, 70–79, and ≥80 had 12.8%, 17.5%, and 49.1% lower odds, respectively (all p<0.05; Figure 1). Patients treated at urban teaching hospitals had 316% higher odds of ablation compared to those at rural hospitals (aOR 4.16; p<0.001).
Conclusion:
Significant disparities exist in the use of catheter ablation for SVT. Female sex, older age, Black race, and Medicaid coverage were associated with lower odds of ablation, while private insurance and care in urban teaching hospitals were associated with higher odds. These findings underscore the need for targeted efforts to address inequities in access to evidence-based electrophysiologic care.
Catheter ablation is a guideline-directed therapy for symptomatic supraventricular tachycardia (SVT), yet disparities in its utilization across patient populations remain inadequately characterized.
Objective:
To evaluate demographic and hospital-level factors associated with catheter ablation among hospitalized patients with SVT in the United States.
Methods:
We analyzed adult hospitalizations with a diagnosis of SVT (ICD-10-CM I47.1) from the National Inpatient Sample (NIS) for the years 2016 through 2020. Catheter ablation was identified using ICD-10-PCS procedure codes. Survey-weighted logistic regression was used to assess associations between demographic characteristics and the odds of receiving ablation. Age was evaluated both as a continuous and categorical variable. Analyses accounted for the complex survey design of the NIS.
Results:
Among approximately 1.87 million weighted hospitalizations for SVT, only 4.1% underwent catheter ablation. Female patients comprised 52.5% of the SVT cohort but had 16.0% lower odds of receiving ablation compared to males (adjusted OR [aOR] 0.84; p<0.001). Black patients had 9.1% lower odds of ablation compared to White patients (aOR 0.91; p=0.002), while Hispanic and Other race groups had 18.1% (aOR 1.18; p<0.001) and 24.6% (aOR 1.25; p=0.003) higher odds, respectively. Insurance status also impacted access: patients with private insurance had 34.2% higher odds of ablation compared to Medicare recipients (aOR 1.34; p<0.001), whereas those with Medicaid had 9.7% lower odds (aOR 0.90; p=0.010). Increasing age was inversely associated with ablation use, with a 1.2% decrease in odds per year of age (aOR 0.99; 95% CI 0.987–0.989; p<0.001). Compared to patients aged 20–29, those aged 40–49 had 15.4% higher odds (aOR 1.15; p=0.018), while patients aged 60–69, 70–79, and ≥80 had 12.8%, 17.5%, and 49.1% lower odds, respectively (all p<0.05; Figure 1). Patients treated at urban teaching hospitals had 316% higher odds of ablation compared to those at rural hospitals (aOR 4.16; p<0.001).
Conclusion:
Significant disparities exist in the use of catheter ablation for SVT. Female sex, older age, Black race, and Medicaid coverage were associated with lower odds of ablation, while private insurance and care in urban teaching hospitals were associated with higher odds. These findings underscore the need for targeted efforts to address inequities in access to evidence-based electrophysiologic care.
More abstracts on this topic:
A Systematic Review and Meta-Analysis on the Anesthetic Approaches for Left Atrial Appendage Occlusion: Comparing Conscious Sedation and General Anesthesia
Zaidi Syed Rafay, Ajmal Umna, Rauf Zainab, Maaz Muhammad, Gulzar Sara, Burki Shahid, Nazir Abubakar, Mirza Azka, Hassan Ahmad, Amir Maaz, Jahangir Muhammad Asad, Rasul Minahil, Raza Muhammad, Malik Mohammad
A new genetic model organism for primate-specific cardiac function and diseaseChang Stephen, Albertelli Megan, Quertermous Thomas, Wright Patricia, Terrien Jeremy, Aujard Fabienne, Wu Joseph, Krasnow Mark, Karanewsky Caitlin, Pendleton Jozeph, Ren Lu, Anzeraey Aude, Froelicher Victor, Liang David, Razafindrakoto Andriamahery, Ravelonjanahary Noeline