Final ID: Su3051
Surgical Outcomes After Delayed Diagnosis of Anomalous Origin of the Left Coronary Artery From the Pulmonary Artery: A Longitudinal Retrospective Study in a National Cardiovascular Center in Peru
Abstract Body (Do not enter title and authors here):
Background: Anomalous origin of the left coronary artery from the pulmonary artery is a rare but potentially fatal congenital anomaly. Timely diagnosis and surgical repair are essential; however, outcome data from low- and middle-income countries remain limited.
Methods: We conducted a retrospective longitudinal observational study at Peru’s national cardiovascular referral center, including pediatric patients diagnosed with anomalous origin of the left coronary artery from the pulmonary artery between 2008 and 2025. Clinical, imaging, surgical, and functional data were collected. The left ventricular ejection fraction (LVEF) was assessed preoperatively, early postoperatively (within the first month), and at the last follow-up. Descriptive and paired analyses were performed.
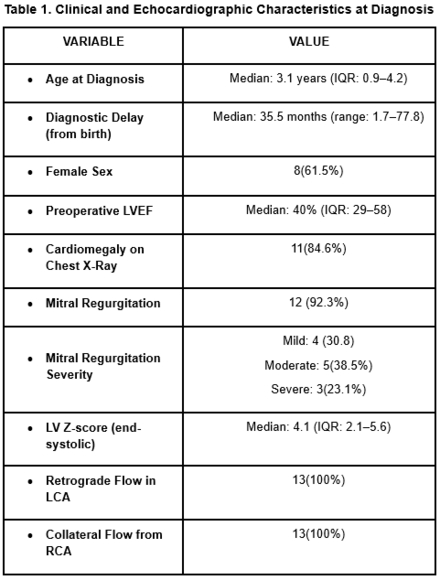
Results: Thirteen patients were included. The median age at diagnosis was 24 months (IQR: 11–50), with 23.1% of cases diagnosed within the first year. The median diagnostic delay from birth was 35 months. Females accounted for 61.5%, and 84.6% were from low-altitude regions (<500 masl). A normal weight-for-age Z-score (−1 to +1) was observed in 53.8% of cases. Dyspnea (61.5%) and diaphoresis (46.2%) were the most common symptoms. A mitral murmur was detected in 92.3% of cases. Pathologic Q waves and T-wave inversion were present in 92.3% and 84.6% of cases, respectively. Cardiomegaly was observed in 84.6% of chest radiographs.
Preoperative echocardiography revealed marked left ventricular dilation (median Z-score: 4.1 systolic, 3.3 diastolic) and reduced LVEF (median: 40%; IQR: 29–58). All patients exhibited retrograde flow in the left coronary artery and collateralization from the right coronary artery.
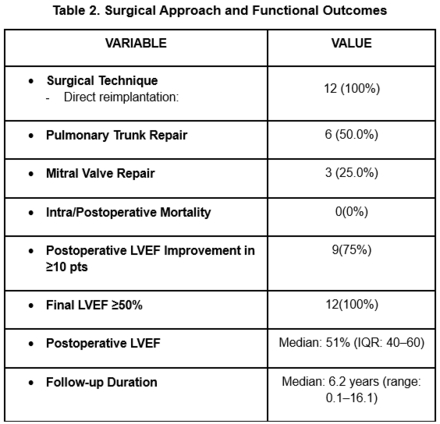
Surgical correction was performed in 12 patients, all of whom underwent direct reimplantation of the left coronary artery. Pulmonary trunk repair was required in 6 cases (50.0%), and mitral valve repair was performed in 3 (25.0%). No perioperative mortality was reported.
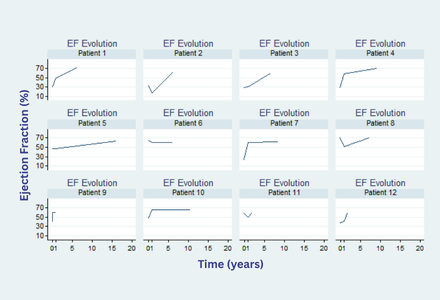
LVEF improved by 10 points or more in 75% of patients. At follow-up (median: 6.2 years; IQR: 1.8–9.2 years), all patients achieved an LVEF of≥50%, with preserved or improved function over time.
Conclusions: In this national cohort, despite delayed diagnosis and initial ventricular dysfunction, surgical correction resulted in complete recovery of ventricular function in all cases, with zero operative mortality.
Background: Anomalous origin of the left coronary artery from the pulmonary artery is a rare but potentially fatal congenital anomaly. Timely diagnosis and surgical repair are essential; however, outcome data from low- and middle-income countries remain limited.
Methods: We conducted a retrospective longitudinal observational study at Peru’s national cardiovascular referral center, including pediatric patients diagnosed with anomalous origin of the left coronary artery from the pulmonary artery between 2008 and 2025. Clinical, imaging, surgical, and functional data were collected. The left ventricular ejection fraction (LVEF) was assessed preoperatively, early postoperatively (within the first month), and at the last follow-up. Descriptive and paired analyses were performed.
Results: Thirteen patients were included. The median age at diagnosis was 24 months (IQR: 11–50), with 23.1% of cases diagnosed within the first year. The median diagnostic delay from birth was 35 months. Females accounted for 61.5%, and 84.6% were from low-altitude regions (<500 masl). A normal weight-for-age Z-score (−1 to +1) was observed in 53.8% of cases. Dyspnea (61.5%) and diaphoresis (46.2%) were the most common symptoms. A mitral murmur was detected in 92.3% of cases. Pathologic Q waves and T-wave inversion were present in 92.3% and 84.6% of cases, respectively. Cardiomegaly was observed in 84.6% of chest radiographs.
Preoperative echocardiography revealed marked left ventricular dilation (median Z-score: 4.1 systolic, 3.3 diastolic) and reduced LVEF (median: 40%; IQR: 29–58). All patients exhibited retrograde flow in the left coronary artery and collateralization from the right coronary artery.
Surgical correction was performed in 12 patients, all of whom underwent direct reimplantation of the left coronary artery. Pulmonary trunk repair was required in 6 cases (50.0%), and mitral valve repair was performed in 3 (25.0%). No perioperative mortality was reported.
LVEF improved by 10 points or more in 75% of patients. At follow-up (median: 6.2 years; IQR: 1.8–9.2 years), all patients achieved an LVEF of≥50%, with preserved or improved function over time.
Conclusions: In this national cohort, despite delayed diagnosis and initial ventricular dysfunction, surgical correction resulted in complete recovery of ventricular function in all cases, with zero operative mortality.
More abstracts on this topic:
A Pressure-Volume Loops Approach Predicts Outcomes After Double Switch Operation For Congenitally Corrected Transposition Of The Great Arteries with Intact Ventricular Septum
Thatte Nikhil, Del Nido Pedro, Ghelani Sunil, Hammer Peter, Marx Gerald, Beroukhim Rebecca, Gauvreau Kimberlee, Callahan Ryan, Prakash Ashwin, Emani Sitaram, Hoganson David
Antithrombotic Strategies and Outcomes in Neonates and Infants with Cardiac Shunts: A Systematic Review and Meta-analysisKiskaddon Amy, Do Nhue, Goldenberg Neil, Betensky Marisol, Branstetter Joshua, Ashour Dina, Williams Pamela, Stock Arabela, Silvey Michael, Giglia Therese