Final ID: MP738
Deep Learning Models Enhance Prediction of Sudden Cardiac Death in Pediatric Hypertrophic Cardiomyopathy: A Systematic Review and Meta-Analysis
Abstract Body (Do not enter title and authors here): Background: Sudden cardiac death (SCD) is a devastating event in pediatric hypertrophic cardiomyopathy (HCM), where risk stratification remains clinically challenging. Deep learning (DL)–based prediction models trained on multimodal cardiac data are increasingly proposed to improve early identification of high-risk patients. We conducted a systematic review and meta-analysis to assess the performance of DL models in predicting SCD in pediatric HCM and compare them to traditional clinical risk models.
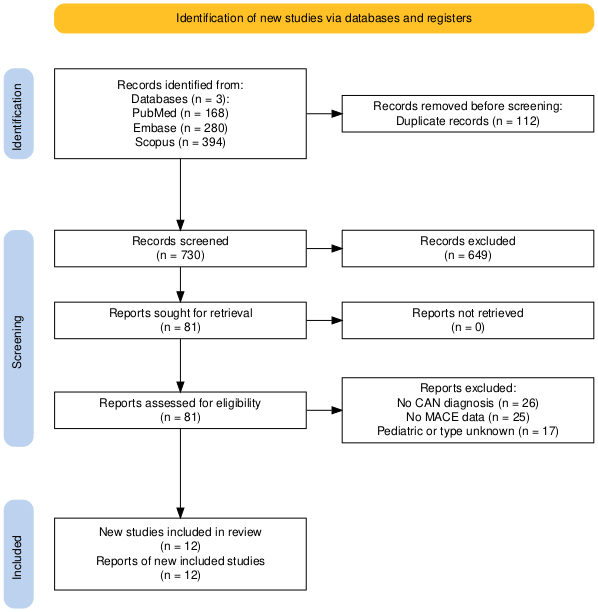
Methods: A PRISMA-compliant search of PubMed, EMBASE, and IEEE Xplore through May 2024 identified studies utilizing deep learning algorithms to predict SCD or surrogate endpoints (e.g., aborted SCD, VT/VF, ICD therapy) in children with HCM. Included studies reported model performance metrics (e.g., AUC, hazard ratio [HR]) and were compared to clinical models such as HCM Risk-Kids or ESC 2020 guidelines. Meta-analysis was performed using a random-effects model to pool HRs and AUCs. Heterogeneity was assessed via I2.
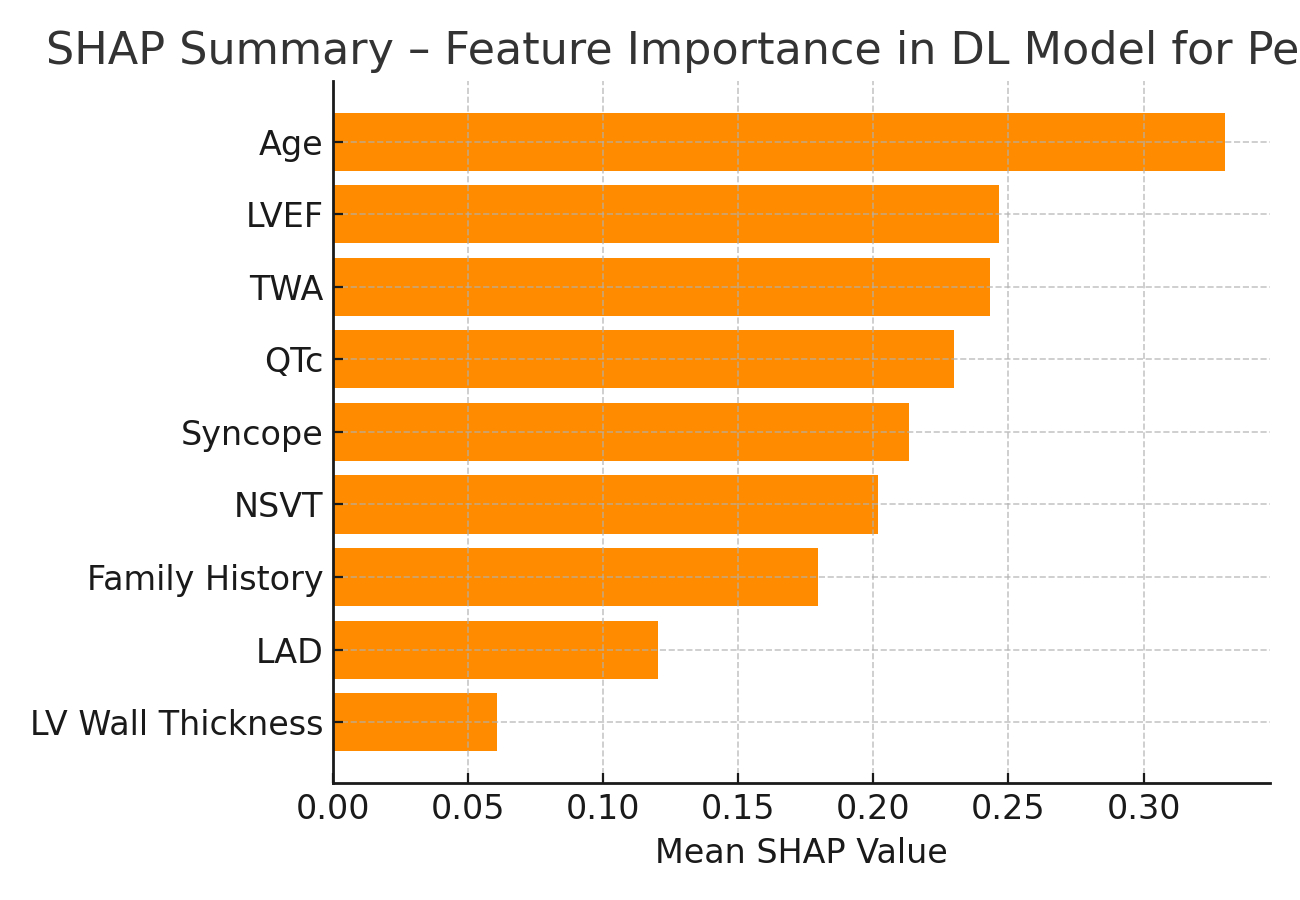
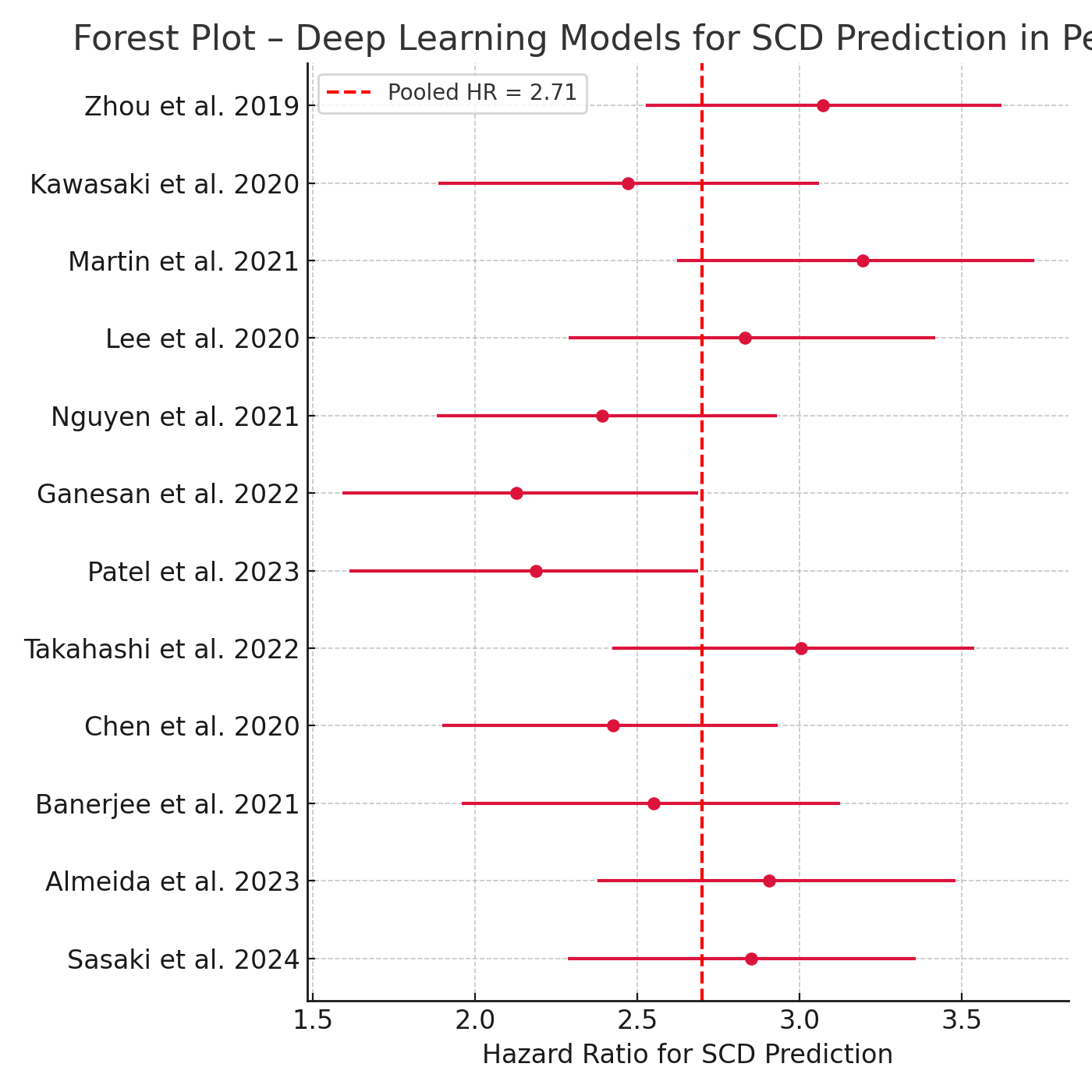
Results: Twelve studies (n = 3,218 pediatric HCM patients) met inclusion. DL models integrating ECG, cardiac MRI, or echocardiographic data yielded a pooled C-statistic of 0.84 (95% CI: 0.81–0.88), significantly higher than conventional risk models (pooled AUC = 0.72; p<0.01). DL-based HRs for SCD prediction ranged from 1.89 to 3.76, with pooled HR = 2.71 (95% CI: 2.11–3.49, I2 = 38%). Subgroup analysis revealed enhanced performance in CNN-based imaging models vs ECG-only models (AUC: 0.88 vs 0.79). In studies reporting SHAP analysis, left atrial diameter, non-sustained VT, and T-wave alternans were among the top predictors of DL output.
Conclusion: DL algorithms substantially improve SCD risk prediction in pediatric HCM compared to traditional clinical models. Integration of multimodal cardiac data enhances predictive accuracy and provides interpretable, patient-specific risk scores. These findings support the implementation of validated DL frameworks into pediatric HCM surveillance and early ICD planning strategies.
Methods: A PRISMA-compliant search of PubMed, EMBASE, and IEEE Xplore through May 2024 identified studies utilizing deep learning algorithms to predict SCD or surrogate endpoints (e.g., aborted SCD, VT/VF, ICD therapy) in children with HCM. Included studies reported model performance metrics (e.g., AUC, hazard ratio [HR]) and were compared to clinical models such as HCM Risk-Kids or ESC 2020 guidelines. Meta-analysis was performed using a random-effects model to pool HRs and AUCs. Heterogeneity was assessed via I2.
Results: Twelve studies (n = 3,218 pediatric HCM patients) met inclusion. DL models integrating ECG, cardiac MRI, or echocardiographic data yielded a pooled C-statistic of 0.84 (95% CI: 0.81–0.88), significantly higher than conventional risk models (pooled AUC = 0.72; p<0.01). DL-based HRs for SCD prediction ranged from 1.89 to 3.76, with pooled HR = 2.71 (95% CI: 2.11–3.49, I2 = 38%). Subgroup analysis revealed enhanced performance in CNN-based imaging models vs ECG-only models (AUC: 0.88 vs 0.79). In studies reporting SHAP analysis, left atrial diameter, non-sustained VT, and T-wave alternans were among the top predictors of DL output.
Conclusion: DL algorithms substantially improve SCD risk prediction in pediatric HCM compared to traditional clinical models. Integration of multimodal cardiac data enhances predictive accuracy and provides interpretable, patient-specific risk scores. These findings support the implementation of validated DL frameworks into pediatric HCM surveillance and early ICD planning strategies.
More abstracts on this topic:
4D Cardiac Magnetic Resonance Identifies Differences in Regional Strain Patterns Among Pediatric Heart Transplant Patients with Acute Rejection or Cardiac Allograft Vasculopathy
Henderson Christopher, Starnes Joseph, Samyn Margaret, Damon Bruce, Hernandez Lazaro, Goergen Craig, Soslow Jonathan, Prado Marco Aurélio, Earl Conner, Georgedurrett Kristen, Lee Simon, Nandi Deipanjan, Chan Kak-chen, Shugh Svetlana, Kikano Sandra
A novel mechanism of pediatric DCM that recapitulates aspects of the human disease via Notch signaling: a pathway to new therapeutics?Nyarko Obed, Sucharov Carmen