Final ID: Sa4031
Familial Clustering of Mital Valve Prolapse and Mitral Valve Regurgitation
Abstract Body (Do not enter title and authors here): Introduction: Studies have found significant familial clustering of mitral valve prolapse (MVP) and mitral valve regurgitation (MVR) in parent-child and sibling studies. However, genetic screening in MVP/MVR patients without syndromic presentation or in their family members is not recommended. Here we extend the familial clustering evidence beyond nuclear families and examine characteristics of MVP/MVR patients from high-risk MVP/MVR pedigrees.
Methods: Transesophageal echocardiograms (ECHO) of patients seen at Intermountain Health from June 2006 to June 2024 were evaluated. Reported severity of MVP/MVR was used to categorize patients as severe, moderate, or mild (mild had to be reported on 2 or more ECHO). Patient characteristics were compared based on MVP/MVR ECHO severity. The Intermountain Genealogy Registry (IGR), a genealogy linked to Intermountain patients, was used to identify MVP/MVR cases from pedigrees. We compared MVP/MVR cases in pedigrees with high rates of MVP/MVR (relative rate >5 times general patient population) to MVP/MVR cases in pedigrees with low rates of MVP/MVR. Finally, the IGR was used for large pedigree (≥3 generations) familial clustering analyses, based on genealogy familial index (GIF), which is the average kinship co-efficient for all case pairs.
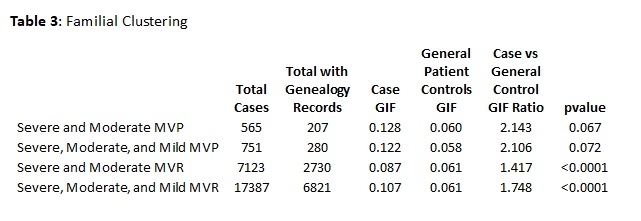
Results: A total of 751 MVP and 17,387 MVR patients were identified from 163,267 ECHOs. Those with severe MVP/MVR disease tended to male and have fewer comorbidities (Table 1). However, only males were significantly more likely to come from high-risk MVP/MVR pedigrees compared to low-risk MVP/MVR pedigrees (Table 2). MVP case pairs from large pedigrees had double the average relatedness (GIF ratio=2.1; Table 3), and while not significant, there was a trend toward different when compared to general patient pairs (p=0.07). However, the MVR case pairs from larger pedigrees did have a significant increase in relatedness (GIF ratio=1.4-1.7) compared to general patient pairs (p<0.0001).
Conclusions: There was no distinguishing patient characteristic, except for male sex, that indicated that an MVP/MVR patient was from a high-risk MVP/MVR pedigree. However, there was a trend toward significant familial clustering in large MVP pedigrees and a significant increase in relatedness for MVR. Examination of ECHO-specific parameters might help determine which ones are associated with MVP/MVR patients most likely from high-risk pedigrees and whose family members might be at higher risk.
Methods: Transesophageal echocardiograms (ECHO) of patients seen at Intermountain Health from June 2006 to June 2024 were evaluated. Reported severity of MVP/MVR was used to categorize patients as severe, moderate, or mild (mild had to be reported on 2 or more ECHO). Patient characteristics were compared based on MVP/MVR ECHO severity. The Intermountain Genealogy Registry (IGR), a genealogy linked to Intermountain patients, was used to identify MVP/MVR cases from pedigrees. We compared MVP/MVR cases in pedigrees with high rates of MVP/MVR (relative rate >5 times general patient population) to MVP/MVR cases in pedigrees with low rates of MVP/MVR. Finally, the IGR was used for large pedigree (≥3 generations) familial clustering analyses, based on genealogy familial index (GIF), which is the average kinship co-efficient for all case pairs.
Results: A total of 751 MVP and 17,387 MVR patients were identified from 163,267 ECHOs. Those with severe MVP/MVR disease tended to male and have fewer comorbidities (Table 1). However, only males were significantly more likely to come from high-risk MVP/MVR pedigrees compared to low-risk MVP/MVR pedigrees (Table 2). MVP case pairs from large pedigrees had double the average relatedness (GIF ratio=2.1; Table 3), and while not significant, there was a trend toward different when compared to general patient pairs (p=0.07). However, the MVR case pairs from larger pedigrees did have a significant increase in relatedness (GIF ratio=1.4-1.7) compared to general patient pairs (p<0.0001).
Conclusions: There was no distinguishing patient characteristic, except for male sex, that indicated that an MVP/MVR patient was from a high-risk MVP/MVR pedigree. However, there was a trend toward significant familial clustering in large MVP pedigrees and a significant increase in relatedness for MVR. Examination of ECHO-specific parameters might help determine which ones are associated with MVP/MVR patients most likely from high-risk pedigrees and whose family members might be at higher risk.
More abstracts on this topic:
Biomechanical Impact of Crossing Neochords In Mitral Valve Repair Using Ex Vivo Mitral Valve Prolapse Models
Zhu Yuanjia, Huynh Chris, Wu Catherine, Park Matthew, Elde Stefan, Yajima Shin, Kim Joon Bum, Woo Y Joseph
A-band titin-truncating variant promotes the development of arrhythmia-induced cardiomyopathy in a novel genetically-engineered porcine modelLee Kwonjae, Del Rio Carlos, Mcnally Elizabeth, Pfenniger Anna, Bhatnagar Ashita, Glinton Kristofor, Burrell Amy, Ober Rebecca, Mcluckie Alicia, Bishop Brian, Rogers Christopher, Geist Gail