Final ID: MP1422
The Risk of Pancreatitis and Adverse Cardiovascular Events in Patients with Type 2 Diabetes and/or Overweight/Obesity with and without Hypertriglyceridemia when Prescribed GLP1RA: A Propensity Score-Matched Analysis
Abstract Body (Do not enter title and authors here): Introduction: Concern for an increased risk of pancreatitis in patients prescribed glucagon-like peptide-1 receptor agonists (GLP1RAs) persists despite the lack of firm causality. Clinicians may therefore be hesitant to prescribe this treatment in patients at higher risk of pancreatitis, such as those with hypertriglyceridemia (HTG). Conversely, GLP-1RAs can positively affect triglyceride (TG) homeostasis and lead to lower plasma TG. This study evaluated whether GLP1RAs were associated with an increased risk of pancreatitis and major adverse cardiovascular events (MACE) in patients with and without HTG.
Methods: We queried the Intermountain Health electronic medical records for patients ≥18 years old from January 2006 to April 2025 with Type 2 diabetes (T2D) and/or body mass index (BMI) ≥27 either on GLP1RA at baseline or never on GLP1RA with measured TG. Propensity score (PS) matching with a greedy nearest neighbor algorithm was used to pair the groups. Using the PS matched pairs, Cox-proportional hazard regressions (unadjusted and adjusted) were used to examine the risk of follow-up pancreatitis and MACE.
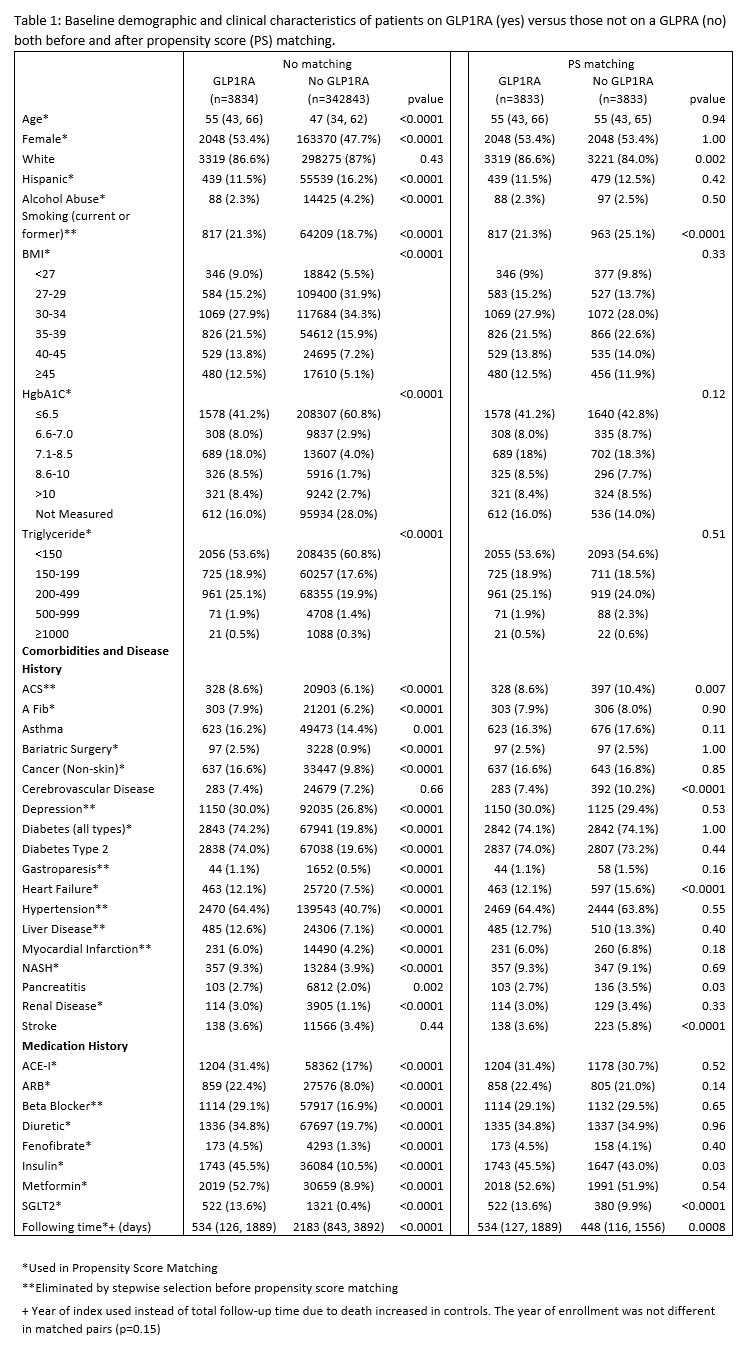
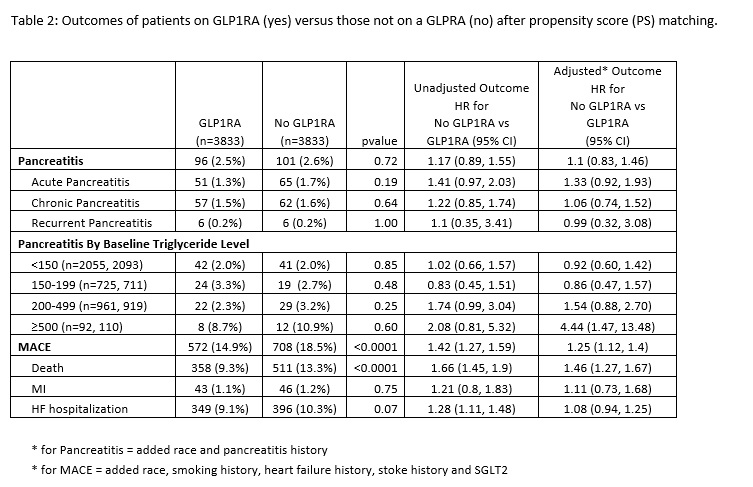
Results: Of the 346,677 patients, 3834 (1.1%) patients were prescribed GPL1RA (342,843 (98.9%) without GLP1RA). Those on a GLP1RA were older, more likely to be non-Hispanic, have lower rates of alcohol abuse and higher BMI, Hgb A1C, and TG, and tended to have more comorbidities and medication use (Table 1). The PS matching resulted in a well-matched cohort of 3833 pairs (Table 1). The rate of pancreatitis was similar in those on GLP1RA compared to those not (2.5% vs 2.6%, p=0.72) (Table 2). The risk of pancreatitis was further examined by baseline TG levels. For patients with severe TG levels (≥500 mg/dL), those on a GLP1RA had a non-significant decrease in pancreatitis (8.7% vs 10.9%, p=0.60); however, after adjustment for prior pancreatitis history the hazard ratio (HR) for pancreatitis was over 4 times greater for those not on GLP1RA vs those on a GLP1RA. MACE events on GLP1RA were also lower (14.9% vs 18.5%, p<0.0001) with MACE HR of 1.25 when not on GLP1RA (Table 2).
Conclusions: These results support findings of prior studies that did not identify an increased risk of pancreatitis in patients prescribed a GLP1RA. Additionally, there was not an increased risk of pancreatitis in patients with HTG, including those with TG ≥ 500 mg/dL. Based on this analysis, prescribers may feel more confident about prescribing GLP1RAs to patients with HTG.
Methods: We queried the Intermountain Health electronic medical records for patients ≥18 years old from January 2006 to April 2025 with Type 2 diabetes (T2D) and/or body mass index (BMI) ≥27 either on GLP1RA at baseline or never on GLP1RA with measured TG. Propensity score (PS) matching with a greedy nearest neighbor algorithm was used to pair the groups. Using the PS matched pairs, Cox-proportional hazard regressions (unadjusted and adjusted) were used to examine the risk of follow-up pancreatitis and MACE.
Results: Of the 346,677 patients, 3834 (1.1%) patients were prescribed GPL1RA (342,843 (98.9%) without GLP1RA). Those on a GLP1RA were older, more likely to be non-Hispanic, have lower rates of alcohol abuse and higher BMI, Hgb A1C, and TG, and tended to have more comorbidities and medication use (Table 1). The PS matching resulted in a well-matched cohort of 3833 pairs (Table 1). The rate of pancreatitis was similar in those on GLP1RA compared to those not (2.5% vs 2.6%, p=0.72) (Table 2). The risk of pancreatitis was further examined by baseline TG levels. For patients with severe TG levels (≥500 mg/dL), those on a GLP1RA had a non-significant decrease in pancreatitis (8.7% vs 10.9%, p=0.60); however, after adjustment for prior pancreatitis history the hazard ratio (HR) for pancreatitis was over 4 times greater for those not on GLP1RA vs those on a GLP1RA. MACE events on GLP1RA were also lower (14.9% vs 18.5%, p<0.0001) with MACE HR of 1.25 when not on GLP1RA (Table 2).
Conclusions: These results support findings of prior studies that did not identify an increased risk of pancreatitis in patients prescribed a GLP1RA. Additionally, there was not an increased risk of pancreatitis in patients with HTG, including those with TG ≥ 500 mg/dL. Based on this analysis, prescribers may feel more confident about prescribing GLP1RAs to patients with HTG.
More abstracts on this topic:
A short version of HFD/L-NAME mouse model enabling time-effective proof of concept studies to evaluate drugs targeting the cardiometabolic and mild hypertension associated HFpEF phenotype.
Assaly Rana, Dubroca Caroline, Waget Aurelie, Perrier Kevin, Sulpice Thierry
Adiposomal microRNAs Mediate Vascular Dysfunction in Obesity-Associated Type 2 DiabetesMirza Imaduddin, Morsy Mohammed, Levitan Irena, Raj Usha, Mahmoud Abeer