Final ID: MP1753
Using Contemporary, Real World Pediatric Pulmonary Hypertension Data to Investigate the Current Treatment Strategies, Survival, and Hospitalization Rates
Abstract Body (Do not enter title and authors here): Background: Presently pediatric pulmonary hypertension (PH) lacks a widely accepted risk assessment algorithm and clear guidelines for treatment. Most targeted therapies are used off-label in pediatrics, and current registries do not capture the full breadth of pediatric PH in the U.S., limiting insight into treatment patterns and outcomes.
Question: How is pediatric PH treated in the U.S. and what is the expected prognosis?
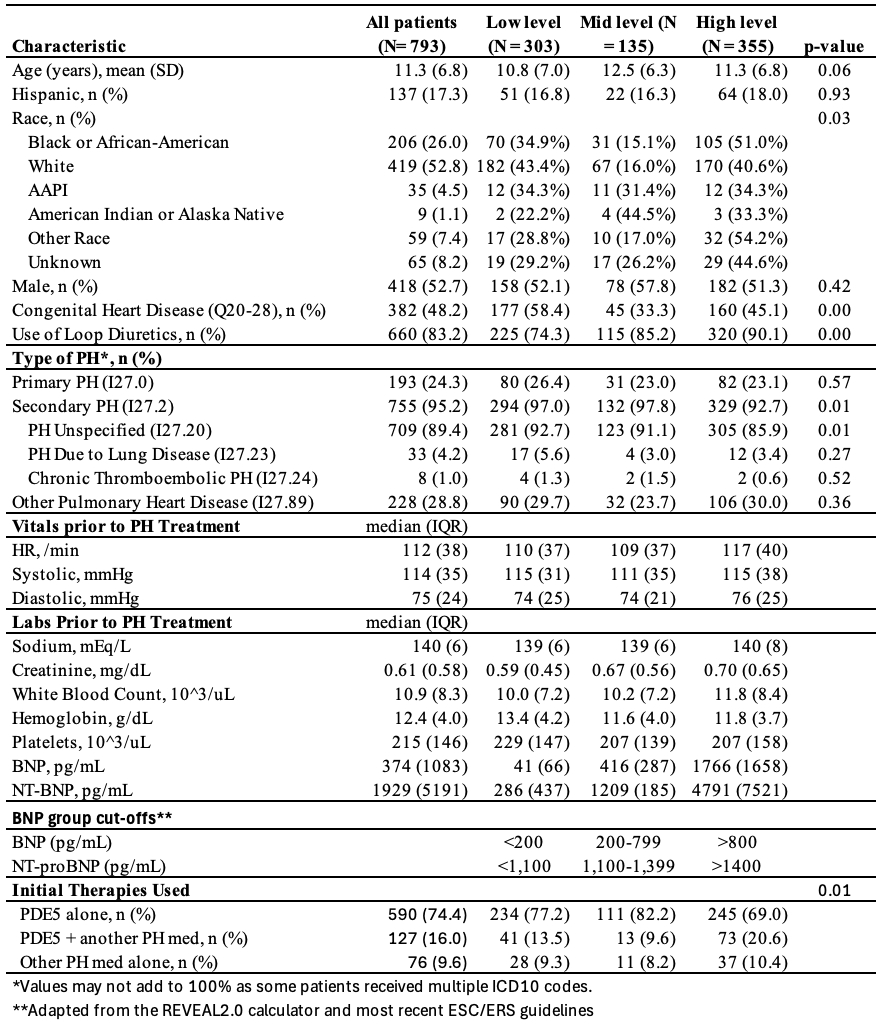
Methods: Patient data were obtained through the TriNetX Research Network, which provides de-identified patient health information from electronic medical records in the US, and we included patients aged 1 to 21 years diagnosed with PH based on ICD10 code, including primary PH and secondary PH, who were treated with targeted PH therapy, and had a pre-treatment BNP/NT-proBNP (BNP) level. Patients were excluded if they were on iNO alone or had PH due to left heart disease. BNP stratification was made through an adaptation of REVEAL 2.0 and recent ESC/ERS guidelines (Table 1). Primary outcomes were death or hospitalizations 1 year after diagnosis.
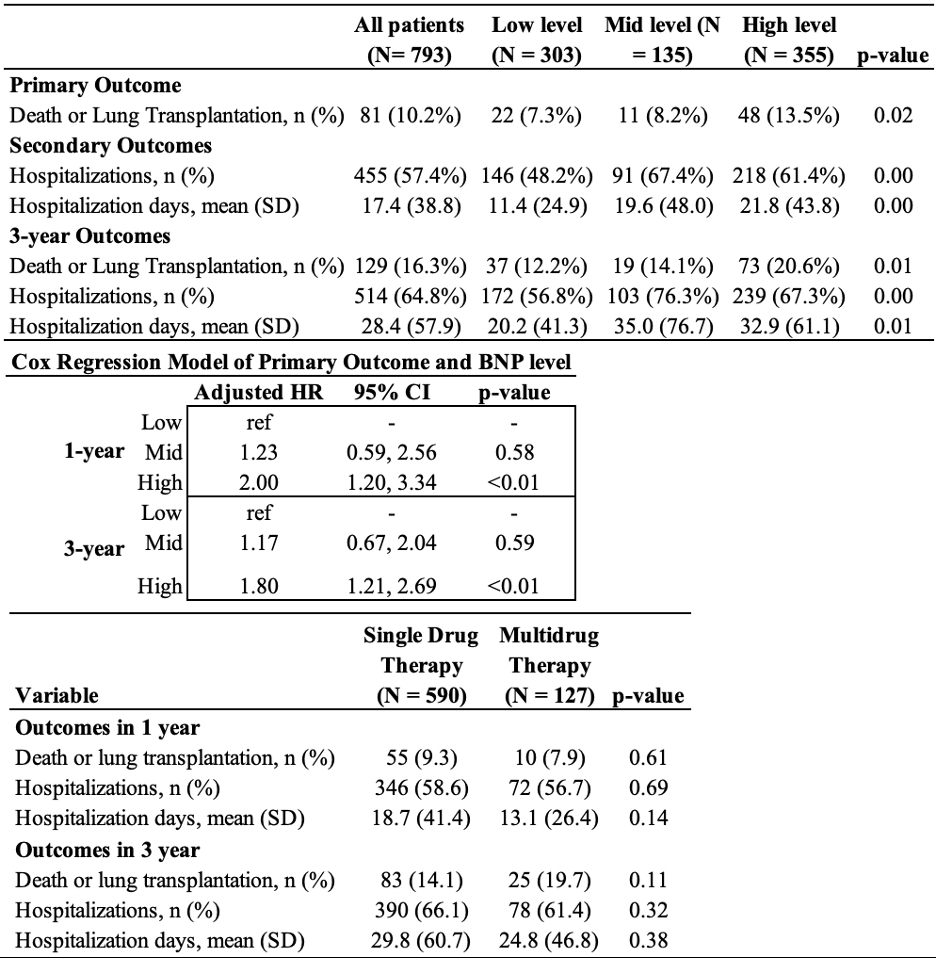
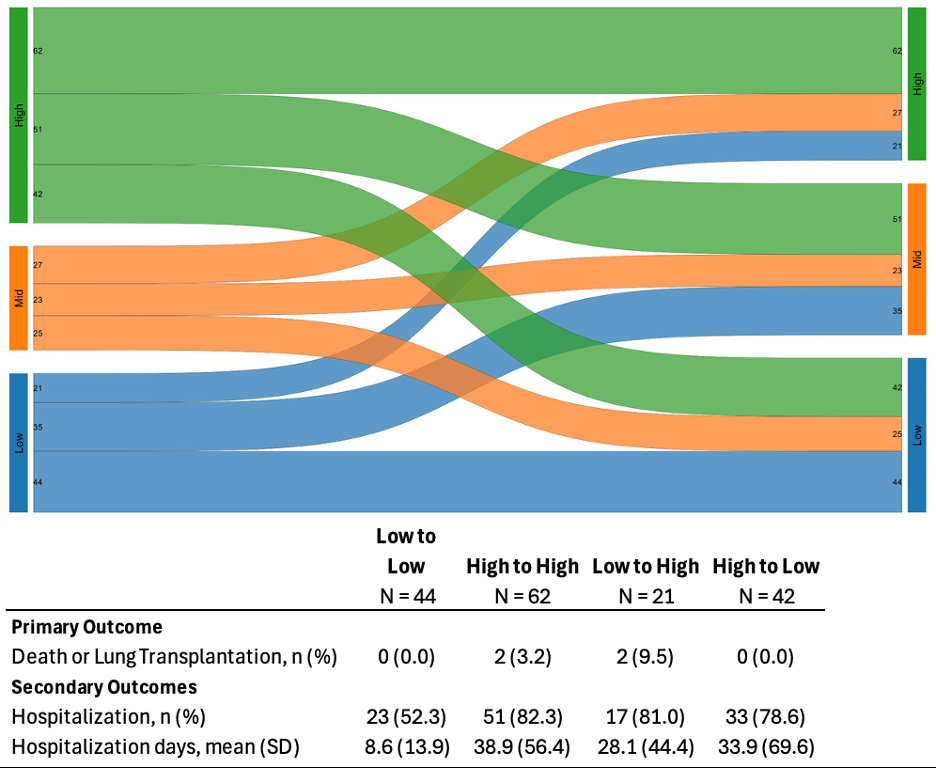
Results: We identified 793 patients who fit the criteria. Pre-treatment BNP levels were grouped “low” (n=303), “mid” (n=135), or “high” (n=355). The cohort was predominately White (n=419) and Black or African-American (BAA) (n=206), with 51% of BAA and 40.6% of White with a high pre-treatment BNP. Initial therapy was predominately a single drug no matter the initial BNP level (low 77.2%, mid 82.2% or high 69%) (Table 1). High BNP levels were a significant predictor of 1- and 3-year survival with a Cox proportional hazard of 2.0 (0.67-2.04, p<0.01) and 1.8 (1.21, 2.69, p<0.01), respectively. When looking at initial treatment intensity, there was no difference in mortality between those who were on single or multi-drug therapy at 1- and 3-years (Table 2). Using a Sankey plot for 1-year post diagnosis trends, roughly a third of each group transitioned to another level, and those who experienced mortality were restricted to mainly those patients who worsened or remained in the high level BNP group (Figure 1).
Conclusion: Mortality was seen in those with initial high BNP levels at 1- and 3- years after diagnosis, but was not significantly different in those who were started on single vs multi-drug therapy. To our knowledge this is the largest cohort of pediatric PH patients looking at the current landscape of pediatric PH, prognostic value of BNP, and current therapy choices and expected outcomes.
Question: How is pediatric PH treated in the U.S. and what is the expected prognosis?
Methods: Patient data were obtained through the TriNetX Research Network, which provides de-identified patient health information from electronic medical records in the US, and we included patients aged 1 to 21 years diagnosed with PH based on ICD10 code, including primary PH and secondary PH, who were treated with targeted PH therapy, and had a pre-treatment BNP/NT-proBNP (BNP) level. Patients were excluded if they were on iNO alone or had PH due to left heart disease. BNP stratification was made through an adaptation of REVEAL 2.0 and recent ESC/ERS guidelines (Table 1). Primary outcomes were death or hospitalizations 1 year after diagnosis.
Results: We identified 793 patients who fit the criteria. Pre-treatment BNP levels were grouped “low” (n=303), “mid” (n=135), or “high” (n=355). The cohort was predominately White (n=419) and Black or African-American (BAA) (n=206), with 51% of BAA and 40.6% of White with a high pre-treatment BNP. Initial therapy was predominately a single drug no matter the initial BNP level (low 77.2%, mid 82.2% or high 69%) (Table 1). High BNP levels were a significant predictor of 1- and 3-year survival with a Cox proportional hazard of 2.0 (0.67-2.04, p<0.01) and 1.8 (1.21, 2.69, p<0.01), respectively. When looking at initial treatment intensity, there was no difference in mortality between those who were on single or multi-drug therapy at 1- and 3-years (Table 2). Using a Sankey plot for 1-year post diagnosis trends, roughly a third of each group transitioned to another level, and those who experienced mortality were restricted to mainly those patients who worsened or remained in the high level BNP group (Figure 1).
Conclusion: Mortality was seen in those with initial high BNP levels at 1- and 3- years after diagnosis, but was not significantly different in those who were started on single vs multi-drug therapy. To our knowledge this is the largest cohort of pediatric PH patients looking at the current landscape of pediatric PH, prognostic value of BNP, and current therapy choices and expected outcomes.
More abstracts on this topic:
A validated metabolite-based biomarker score for fruit and vegetable intake and associations with all-cause mortality and incident cardiometabolic diseases
Oude Griep Linda, Li Chunxiao, Koulman Albert, Imamura Fumiaki, Wareham Nicholas, Forouhi Nita
A Tense Race: Correlation of Liver Stiffness with Ultrasound Elastography and Hemodynamics in Fontan Patients.Lo Yau Yuen, Purlee Matthew, Brinkley Lindsey, Gupta Dipankar, Lopez-colon Dalia, Saulino David, Coppola John Anthony, Vyas Himesh