Final ID: MP389
Mapping Inequity: Racial Disparities and Social Vulnerability Drive Sudden Cardiac Death Hotspots Across U.S. Counties
Abstract Body (Do not enter title and authors here):
Background
Sudden cardiac death (SCD) is a leading cause of mortality in the U.S., with emerging evidence pointing to racial disparities and the impact of social vulnerability. Yet, geographic patterns integrating race and county-level vulnerability remain underexplored.
Objective
To identify U.S. counties where socially vulnerable communities, stratified by race/ethnicity, experience disproportionate burdens of SCD-related mortality.
Methods
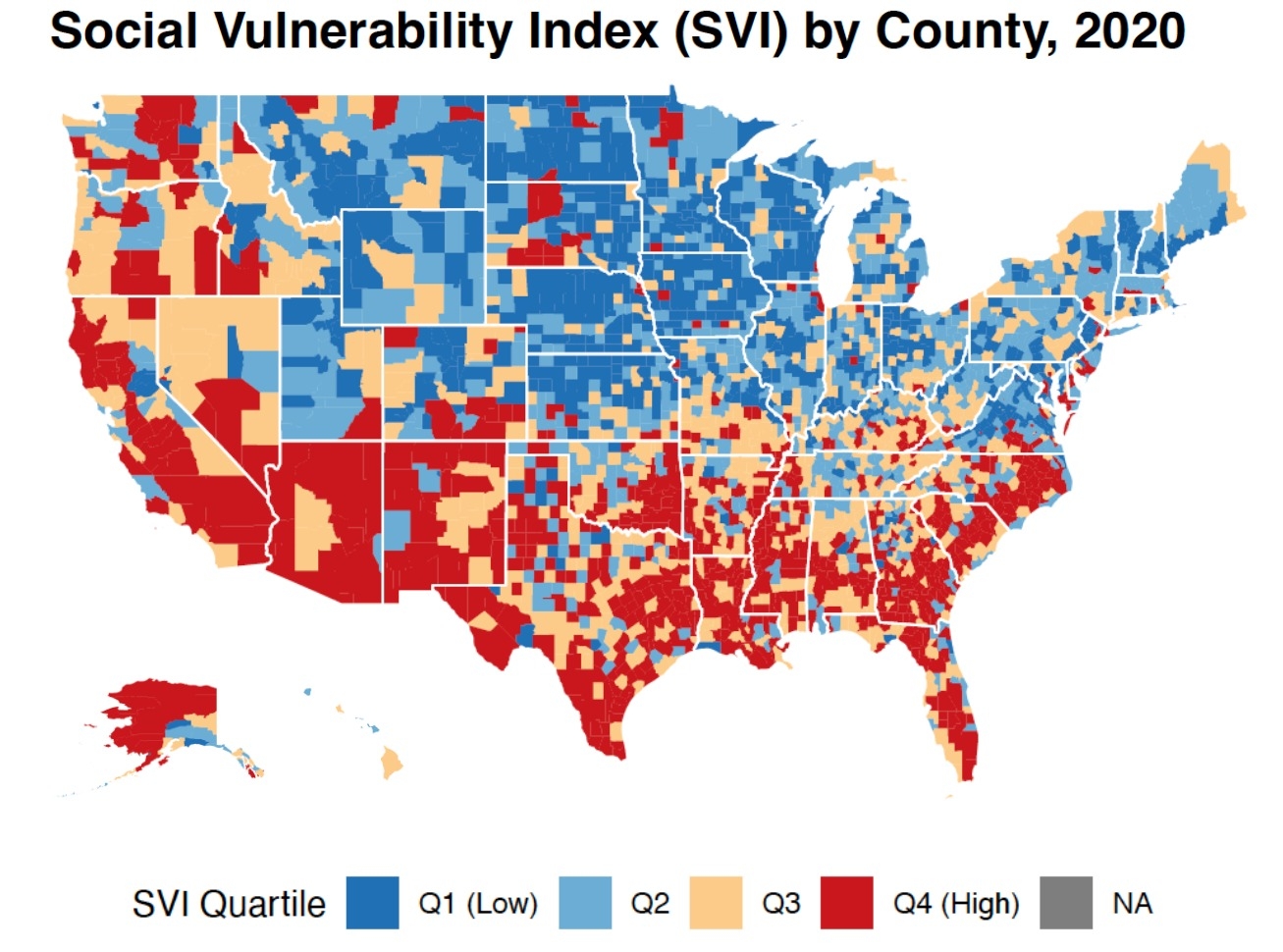
We analyzed county-level data (1999-2020), integrating age-adjusted mortality rates (AAMR) for SCD with the 2020 CDC Social Vulnerability Index (SVI). Counties were categorized into SVI quartiles (Q1: Low to Q4: High Social Vulnerability). Analyses were stratified by race/ethnicity: Black or African American, Hispanic/Latino, White, American Indian/Alaska Native (AI/AN), and Asian/Pacific Islander (API). We used RStudio (v2023.06.1) for data cleaning, ANOVA testing, and descriptive analysis. “Unreliable” mortality values were handled as missing or set to zero, with only valid AAMR > 0 included. Hotspot counties were identified by selecting the top decile of AAMR SCD within Q4 SVI counties.
Results
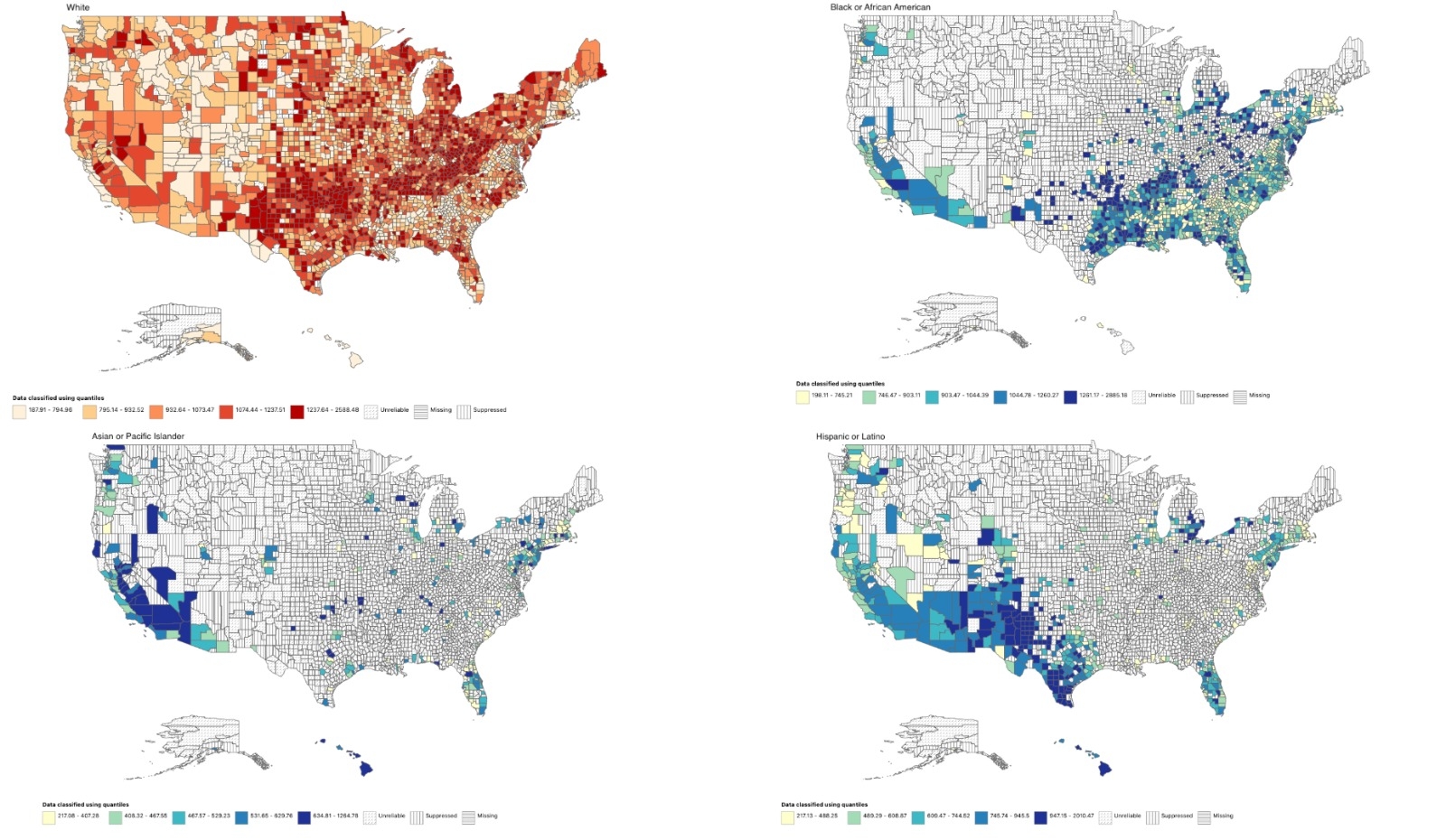
Significant disparities emerged across SVI quartiles for Black (p = 0.0003), Hispanic (p < 0.0001), and White (p < 0.0001) groups. Mean AAMR more than doubled from low to high SVI counties in Black communities (17.0 to 39.4 per 100,000). White and Hispanic groups showed smaller but consistent increases. API (p = 0.60) or AI/AN (p = 0.63) groups showed no significant trends. Madison Parish, LA appeared in the top-10 highest-burden counties across all groups. Black populations faced extreme rates in some SVI counties (e.g., Madison Parish, LA: 351.4 per 100,000), while API groups had low AAMR even in vulnerable areas. Data misclassification limited interpretation in the Hispanic group.
Conclusions
Black, Hispanic, and White populations showed significant differences in SCD mortality tied to social vulnerability. Black populations in the most vulnerable areas experienced more than twice the rate of mortality compared to those in less vulnerable areas, suggesting a strong correlation between social vulnerability and SCD mortality in Black communities. API and AI/AN groups showed no significant associations, likely due to small sample sizes. Madison Parish, LA reflects the compounded impact of structural disadvantage. Findings support targeted interventions in socially and racially vulnerable counties to reduce preventable cardiac deaths.
Background
Sudden cardiac death (SCD) is a leading cause of mortality in the U.S., with emerging evidence pointing to racial disparities and the impact of social vulnerability. Yet, geographic patterns integrating race and county-level vulnerability remain underexplored.
Objective
To identify U.S. counties where socially vulnerable communities, stratified by race/ethnicity, experience disproportionate burdens of SCD-related mortality.
Methods
We analyzed county-level data (1999-2020), integrating age-adjusted mortality rates (AAMR) for SCD with the 2020 CDC Social Vulnerability Index (SVI). Counties were categorized into SVI quartiles (Q1: Low to Q4: High Social Vulnerability). Analyses were stratified by race/ethnicity: Black or African American, Hispanic/Latino, White, American Indian/Alaska Native (AI/AN), and Asian/Pacific Islander (API). We used RStudio (v2023.06.1) for data cleaning, ANOVA testing, and descriptive analysis. “Unreliable” mortality values were handled as missing or set to zero, with only valid AAMR > 0 included. Hotspot counties were identified by selecting the top decile of AAMR SCD within Q4 SVI counties.
Results
Significant disparities emerged across SVI quartiles for Black (p = 0.0003), Hispanic (p < 0.0001), and White (p < 0.0001) groups. Mean AAMR more than doubled from low to high SVI counties in Black communities (17.0 to 39.4 per 100,000). White and Hispanic groups showed smaller but consistent increases. API (p = 0.60) or AI/AN (p = 0.63) groups showed no significant trends. Madison Parish, LA appeared in the top-10 highest-burden counties across all groups. Black populations faced extreme rates in some SVI counties (e.g., Madison Parish, LA: 351.4 per 100,000), while API groups had low AAMR even in vulnerable areas. Data misclassification limited interpretation in the Hispanic group.
Conclusions
Black, Hispanic, and White populations showed significant differences in SCD mortality tied to social vulnerability. Black populations in the most vulnerable areas experienced more than twice the rate of mortality compared to those in less vulnerable areas, suggesting a strong correlation between social vulnerability and SCD mortality in Black communities. API and AI/AN groups showed no significant associations, likely due to small sample sizes. Madison Parish, LA reflects the compounded impact of structural disadvantage. Findings support targeted interventions in socially and racially vulnerable counties to reduce preventable cardiac deaths.
More abstracts on this topic:
Acute Exposure to High PM2.5 Levels Increases the Risk of Late All-Cause Mortality in Patients with STEMI
Fathieh Sina, Tran Hao, Faour Amir, Pahn Reece, Long Mitchell, Tam Gladys, Figtree Gemma, Negishi Kazuaki, French John
10-Year Trends in Last Known Well to Arrival Time in Acute Ischemic Stroke Patients: 2014-2023Ferrone Nicholas, Sanmartin Maria, O'hara Joseph, Jimenez Jean, Ferrone Sophia, Wang Jason, Katz Jeffrey, Sanelli Pina