Final ID: Sa2027
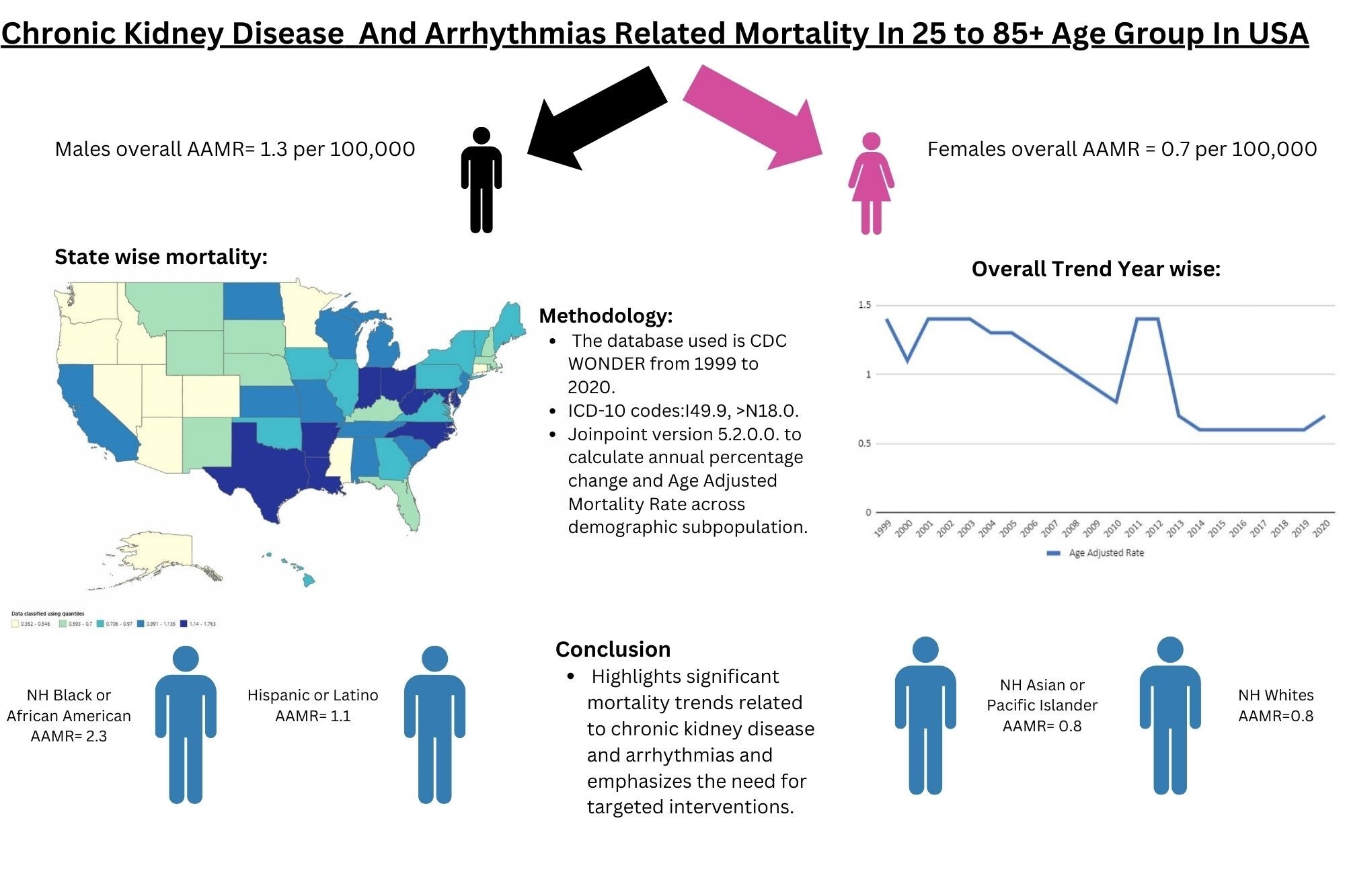
A Retrospective Analysis of Chronic Kidney Disease and Arrhythmias-Related Mortality Among Adults in the United States (1999-2020): Insights into Disparities by Gender, Race/Ethnicity, and Geography
Abstract Body (Do not enter title and authors here): Introduction
Chronic kidney disease (CKD) is strongly linked to fatal cardiac arrhythmias and continues to be a significant health concern in the United States. CKD presents a complex interplay of cardiovascular and non-cardiovascular complications, contributing to significant morbidity and mortality. This study aims to assess disparities and temporal trends in CKD-related arrhythmia mortality to inform targeted interventions.
Methods
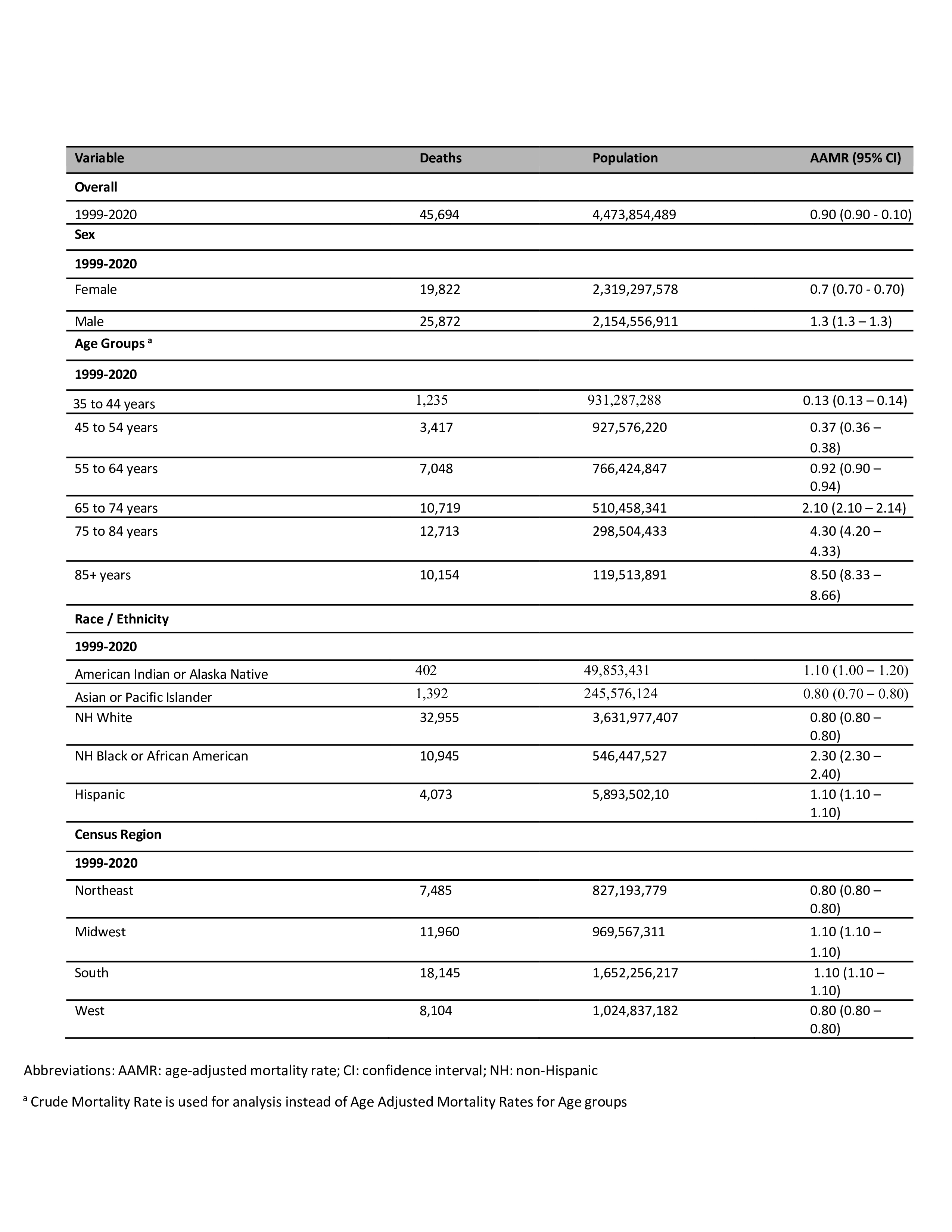
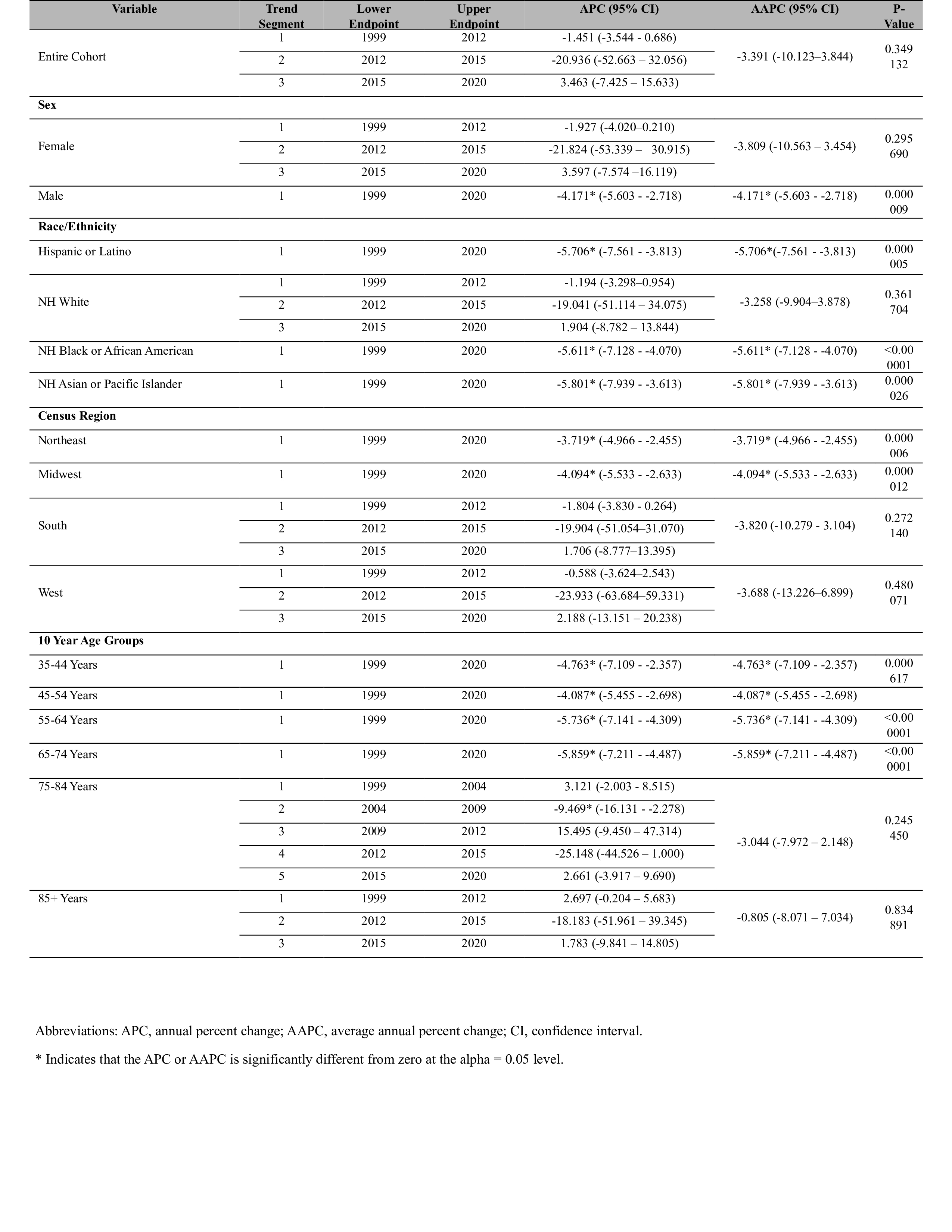
We utilized the International Classification of Diseases (ICD)-10 codes: I49.9, N18.0, N18.1, N18.2, N18.3, N18.4, N18.5, N18.8, N18.9 to extract CKD and Arrhythmias-related mortality data from the CDC WONDER database for individuals aged 25 to 85+ years in the US. Age-adjusted mortality rates (AAMR) were extracted and stratified according to gender, race, and geographic location. Trends in AAMRs were studied by calculating annual percentage change (APC) via Joinpoint regression (Joinpoint Regression Program V 5.2.0).
Results
A total of 45,694 deaths related to CKD and arrhythmia were reported. The overall AAMR was 0.9 (95% CI: 0.9–0.9); males had nearly twice the burden (1.3; 95% CI: 1.3–1.3) compared to females (0.7; 95% CI: 0.7–0.7). AAMR across the study population declined from 1999–2012 (APC -1.45; 95% CI: -3.54 to 0.69), dropped sharply from 2012–2015 (APC -20.94; 95% CI: -52.66 to 32.06), and rose again during 2015–2020 (APC 3.46; 95% CI: -7.43 to 15.63). The steepest decline by age was seen in the 65–74 age group (APC -5.86; 95% CI: -7.21 to -4.49). NH Black individuals bore the highest burden (AAMR 2.3; 95% CI: 2.3–2.4), followed by Hispanic (1.1; 95% CI: 1.1–1.1), NH White (0.8; 95% CI: 0.8–0.8), and NH Asian/Pacific Islander adults (0.8; 95% CI: 0.7–0.8). Regionally, the Midwest showed a consistent decline, while the South and West had a nadir in 2012–2015 followed by a rebound (e.g., South 2015–2020 APC: 1.706; 95% CI: -8.78 to 13.40). State-level AAMRs ranged from highs in Ohio (1.76), DC (1.74), and Texas (1.5) to lows in Alaska (0.46), Colorado (0.39), and Utah (0.35).
Conclusion
Although CKD- and arrhythmia-related mortality declined for much of the study period, the recent uptrend since 2015—driven chiefly by male, NH Black, and Southern populations—signals a resurgence that threatens progress. Targeted interventions addressing sex-, race-, and region-specific drivers are urgently needed to sustain and extend mortality reductions in this high-risk cohort.
Chronic kidney disease (CKD) is strongly linked to fatal cardiac arrhythmias and continues to be a significant health concern in the United States. CKD presents a complex interplay of cardiovascular and non-cardiovascular complications, contributing to significant morbidity and mortality. This study aims to assess disparities and temporal trends in CKD-related arrhythmia mortality to inform targeted interventions.
Methods
We utilized the International Classification of Diseases (ICD)-10 codes: I49.9, N18.0, N18.1, N18.2, N18.3, N18.4, N18.5, N18.8, N18.9 to extract CKD and Arrhythmias-related mortality data from the CDC WONDER database for individuals aged 25 to 85+ years in the US. Age-adjusted mortality rates (AAMR) were extracted and stratified according to gender, race, and geographic location. Trends in AAMRs were studied by calculating annual percentage change (APC) via Joinpoint regression (Joinpoint Regression Program V 5.2.0).
Results
A total of 45,694 deaths related to CKD and arrhythmia were reported. The overall AAMR was 0.9 (95% CI: 0.9–0.9); males had nearly twice the burden (1.3; 95% CI: 1.3–1.3) compared to females (0.7; 95% CI: 0.7–0.7). AAMR across the study population declined from 1999–2012 (APC -1.45; 95% CI: -3.54 to 0.69), dropped sharply from 2012–2015 (APC -20.94; 95% CI: -52.66 to 32.06), and rose again during 2015–2020 (APC 3.46; 95% CI: -7.43 to 15.63). The steepest decline by age was seen in the 65–74 age group (APC -5.86; 95% CI: -7.21 to -4.49). NH Black individuals bore the highest burden (AAMR 2.3; 95% CI: 2.3–2.4), followed by Hispanic (1.1; 95% CI: 1.1–1.1), NH White (0.8; 95% CI: 0.8–0.8), and NH Asian/Pacific Islander adults (0.8; 95% CI: 0.7–0.8). Regionally, the Midwest showed a consistent decline, while the South and West had a nadir in 2012–2015 followed by a rebound (e.g., South 2015–2020 APC: 1.706; 95% CI: -8.78 to 13.40). State-level AAMRs ranged from highs in Ohio (1.76), DC (1.74), and Texas (1.5) to lows in Alaska (0.46), Colorado (0.39), and Utah (0.35).
Conclusion
Although CKD- and arrhythmia-related mortality declined for much of the study period, the recent uptrend since 2015—driven chiefly by male, NH Black, and Southern populations—signals a resurgence that threatens progress. Targeted interventions addressing sex-, race-, and region-specific drivers are urgently needed to sustain and extend mortality reductions in this high-risk cohort.
More abstracts on this topic:
Barriers and Facilitators to Outpatient Cardiac Rehabilitation Attendance Among Patients with Low Socioeconomic Status: A Qualitative Study
Mathews Lena, Okonkwo Miriam Chiamaka, Tolefree Tionna, Stewart Kerry, Benz Scott Lisa, Cooper Lisa, Ndumele Chiadi, Matsushita Kunihiro, Riekert Kristin
Accelerometer-Measured Sedentary Behavior and Future Cardiovascular DiseaseAjufo Ezimamaka, Kany Shinwan, Ramo Joel, Churchill Timothy, Guseh James, Aragam Krishna, Ellinor Patrick, Khurshid Shaan