Final ID: Mo1040
Impact of Frailty on In-Hospital Outcomes for Patients Admitted for Hypertensive Emergency in the United States
Abstract Body (Do not enter title and authors here): Background: Hypertensive emergency (HE) is a life-threatening condition that poses a significant risk for increased morbidity and mortality. It is not known with certainty how a state of declining health, namely with frailty, affects in-hospital outcomes for patients admitted for HE. Herein, we aim to quantify the impact of frailty on in-hospital outcomes for adults admitted for HE and determine whether this association remains consistent across all adult age groups.
Methods: Retrospective analysis was conducted using the National Inpatient Sample database from 2016 to 2022 with STATA18 statistical software. ICD-10 codes were used to identify patients with a primary diagnosis of HE and age at admission. Frailty was assessed using the Hospital Frailty Risk Score, with a score >5 indicating frailty. Multivariate logistic and linear regression analysis was performed to calculate adjusted odds ratios (aOR) while accounting for covariates. The impact of frailty was analyzed for all adults admitted with HE, with subgroup analyses performed for younger (<65 years) and older (≥65 years) patients.
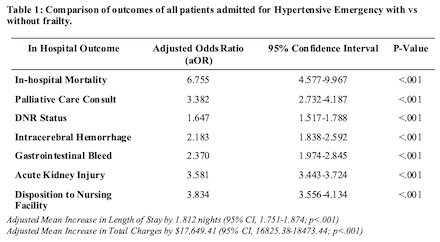
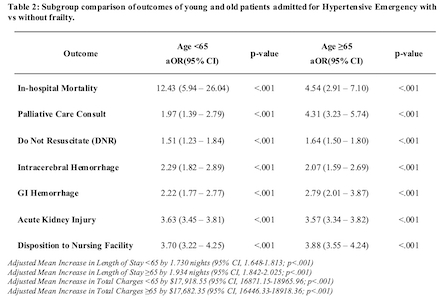
Results: Out of 337,335 patients admitted for HE, 48.6% were classified as frail and 51.4% classified as non-frail. The frail group had a higher average age (60.23 vs 57.93; p<.001) and were predominantly female (53% vs 47%; p<.001). Logistic regression showed frail patients had a significantly higher risk of in-hospital mortality (aOR 6.755, CI 4.577-9.967, p<.001), where similar trends can be seen for additional outcomes such as intracerebral hemorrhage, acute kidney injury, and GI hemorrhage demonstrated in Table 1. Moreover, linear regression showed frail patients experienced an increased adjusted mean length of stay by 1.812 nights (95% CI, 1.751-1.874; p<.001) and higher adjusted mean total charges by $17,649.41 (95% CI, 16,825.38-18,473.44; p<.001). Subgroup analysis stratified by age 65 demonstrated that frailty was still significantly associated with worse outcomes in both age groups (Table 2).
Conclusion: Clinical outcomes are significantly worse with higher resource utilization in frail patients versus non-frail patients admitted for HE. This study demonstrates that the impact of frailty transcends chronological age and challenges the notion that frailty is limited to geriatric populations. Clinicians should be vigilant about assessing the role of frailty in HE to gain crucial clinical insight to enhance patient well-being and appropriate resource allocation.
Methods: Retrospective analysis was conducted using the National Inpatient Sample database from 2016 to 2022 with STATA18 statistical software. ICD-10 codes were used to identify patients with a primary diagnosis of HE and age at admission. Frailty was assessed using the Hospital Frailty Risk Score, with a score >5 indicating frailty. Multivariate logistic and linear regression analysis was performed to calculate adjusted odds ratios (aOR) while accounting for covariates. The impact of frailty was analyzed for all adults admitted with HE, with subgroup analyses performed for younger (<65 years) and older (≥65 years) patients.
Results: Out of 337,335 patients admitted for HE, 48.6% were classified as frail and 51.4% classified as non-frail. The frail group had a higher average age (60.23 vs 57.93; p<.001) and were predominantly female (53% vs 47%; p<.001). Logistic regression showed frail patients had a significantly higher risk of in-hospital mortality (aOR 6.755, CI 4.577-9.967, p<.001), where similar trends can be seen for additional outcomes such as intracerebral hemorrhage, acute kidney injury, and GI hemorrhage demonstrated in Table 1. Moreover, linear regression showed frail patients experienced an increased adjusted mean length of stay by 1.812 nights (95% CI, 1.751-1.874; p<.001) and higher adjusted mean total charges by $17,649.41 (95% CI, 16,825.38-18,473.44; p<.001). Subgroup analysis stratified by age 65 demonstrated that frailty was still significantly associated with worse outcomes in both age groups (Table 2).
Conclusion: Clinical outcomes are significantly worse with higher resource utilization in frail patients versus non-frail patients admitted for HE. This study demonstrates that the impact of frailty transcends chronological age and challenges the notion that frailty is limited to geriatric populations. Clinicians should be vigilant about assessing the role of frailty in HE to gain crucial clinical insight to enhance patient well-being and appropriate resource allocation.
More abstracts on this topic:
2-Methoxyestradiol By Inhibiting Central Action of 12S-Hydroxyeicosatetraenoic Acid Protects Ovariectomized Mice From Hypertension
Dutta Shubha, Singh Purnima, Song Chi Young, Shin Ji Soo, Malik Kafait
A major effect of aprocitentan on albuminuria in patients with resistant hypertensionSchlaich Markus, Bakris George, Flack John, Gimona Alberto, Narkiewicz Krzysztof, Sassi-sayadi Mouna, Wang Jiguang, Weber Michael