Final ID: MP33
The effect of Remote Ischemic Conditioning in Acute Ischemic Stroke Treated with Intravenous Thrombolysis, systematic review and meta analysis
Abstract Body (Do not enter title and authors here): Background:
Intravenous thrombolysis (IVT) improves outcomes in acute ischemic stroke (AIS), but many patients still do not achieve full recovery. Remote ischemic conditioning (RIC) repetitive brief limb ischemia followed by reperfusion, is a low cost, noninvasive strategy that may activate systematic neuroprotective pathways to reduce ischemic reperfusion injury.
Method:
We systematically searched Embase, PubMed, cochrane library, Ovid MEDLINE, Scopus, Web of Science from inception through April 2025, and meta-analysis using RevMan5.4.1. Eligible studies were randomized control trials (RCTs) comparing RIC plus IVT versus IVT with control in patients with AIS. primary outcomes were 90 days modified Rankin Scale (mRS) scores 0–1 and 0–2, stroke recurrence and all-cause mortality. Secondary outcomes hemorrhagic transformation of infarction (HTI), Barthel Index, and NIHSS scores at multiple time points. Random-effects models were used to estimate pooled risk ratios (RR) or mean differences (MD) with 95% confidence intervals (CI) and heterogeneity was assessed with the I2 statistic.
Result:
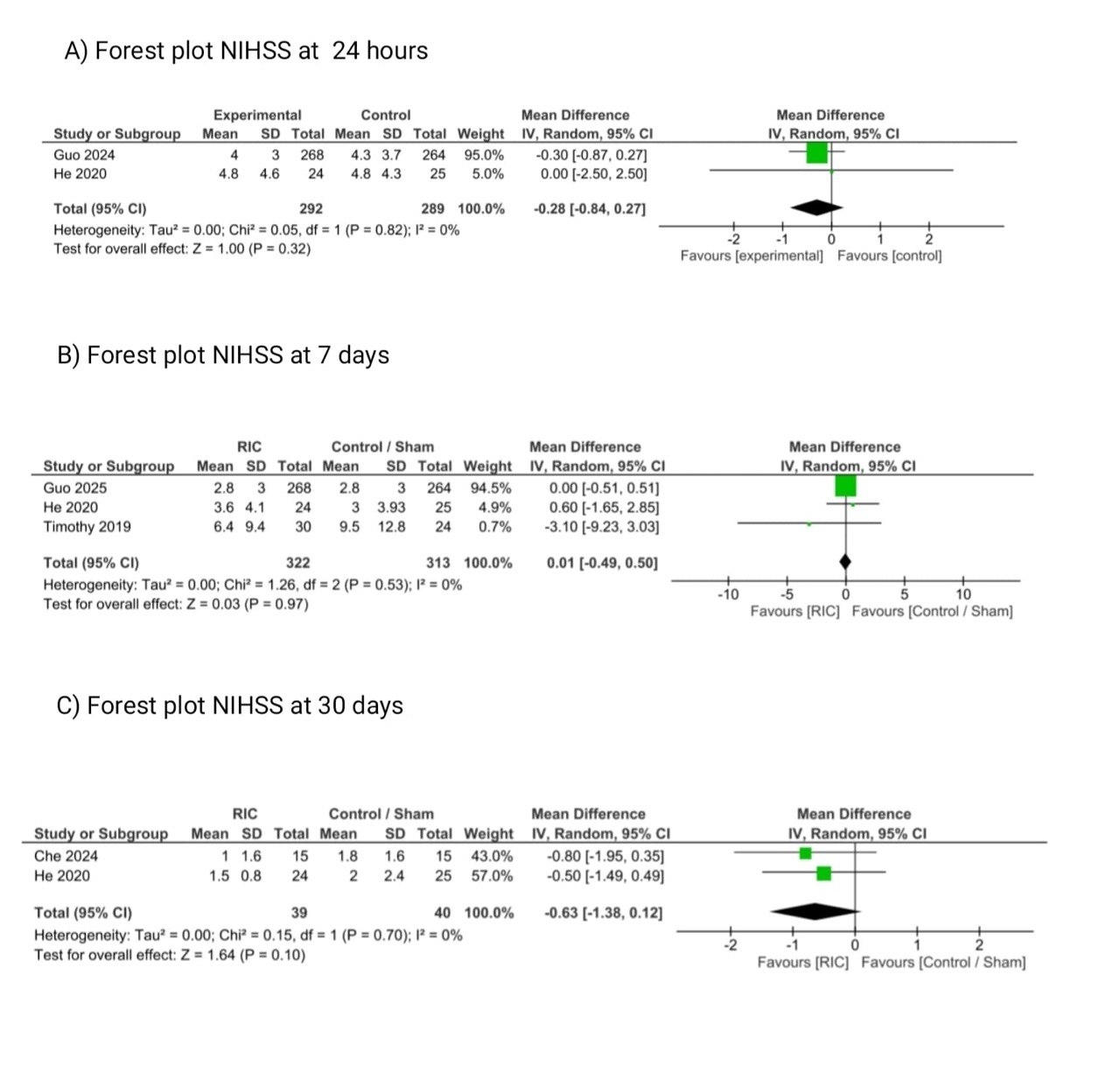
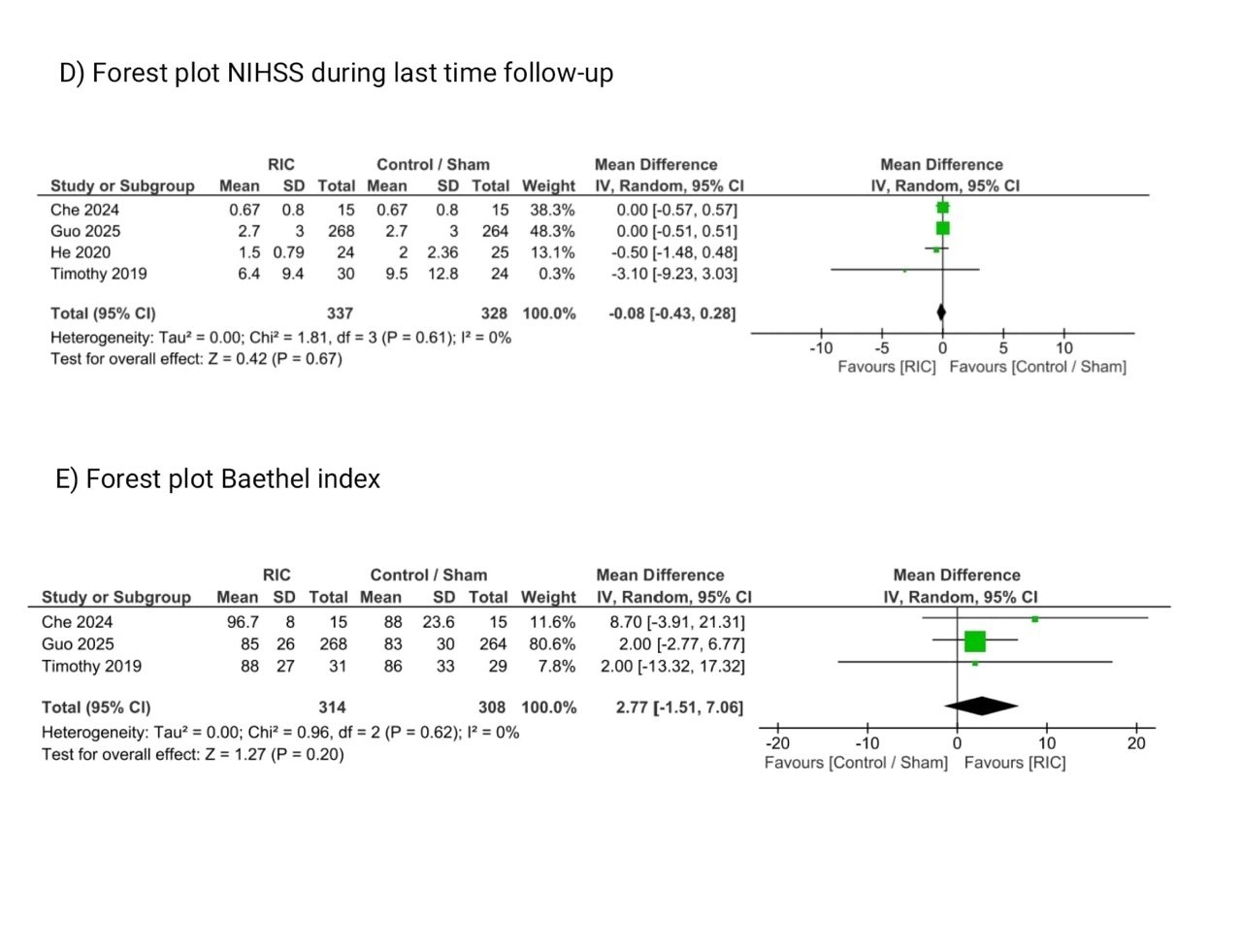
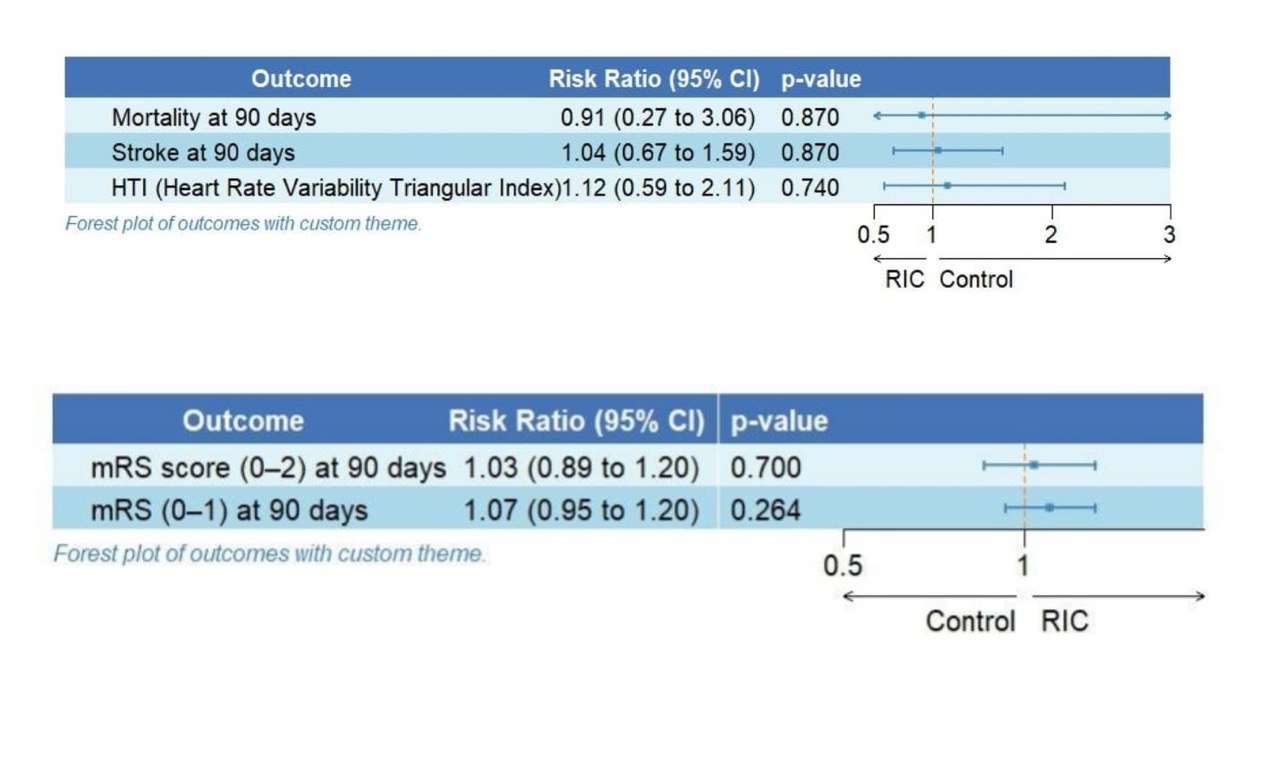
From six studies, a total of 955 patients were included (remote ischemic conditioning [RIC] group: n = 502; sham/control group: n = 453). At 90 days, RIC was not associated with improved functional outcomes: mRS 0–1 (4 studies; RR 1.07, 95% CI 0.95–1.20; p = 0.26; I2 = 17%) or mRS 0–2 (4 studies; RR 1.03, 95% CI 0.89–1.03; p = 0.92; I2 = 64%). Stroke recurrence (4 studies; RR 1.04, 95% CI 0.67–1.59; p = 0.87; I2 = 0%), mortality (3 studies; RR 0.91, 95% CI 0.27–3.06; p = 0.87; I2 = 46%), HTI (3 studies; RR 1.12, 95% CI 0.59–2.11; p = 0.74; I2 = 0%), and Barthel Index (3 studies; MD 2.77, 95% CI –1.51 to 7.06; p = 0.20; I2 = 0%) showed no significant benefit with RIC. NIHSS scores were also comparable at 24 hours (2 studies; MD –0.28, 95% CI –0.84 to 0.27; p = 0.32), 7 days (3 studies; MD 0.01, 95% CI –0.49 to 0.50; p = 0.97), 30 days (2 studies; MD –0.63, 95% CI –1.38 to 0.12; p = 0.10), and last follow-up last follow-up (4 studies; MD –0.08, 95% CI –0.43 to 0.28; p = 0.67), all with I2 = 0%.
Conclusion:
This meta-analysis suggests patients with acute ischemic stroke treated with intravenous thrombolysis and remote ischemic conditioning (RIC) did not significantly improve functional outcomes, reduce stroke recurrence, mortality, or hemorrhagic transformation. No meaningful differences were observed in neurological recovery or activities of daily living.
Intravenous thrombolysis (IVT) improves outcomes in acute ischemic stroke (AIS), but many patients still do not achieve full recovery. Remote ischemic conditioning (RIC) repetitive brief limb ischemia followed by reperfusion, is a low cost, noninvasive strategy that may activate systematic neuroprotective pathways to reduce ischemic reperfusion injury.
Method:
We systematically searched Embase, PubMed, cochrane library, Ovid MEDLINE, Scopus, Web of Science from inception through April 2025, and meta-analysis using RevMan5.4.1. Eligible studies were randomized control trials (RCTs) comparing RIC plus IVT versus IVT with control in patients with AIS. primary outcomes were 90 days modified Rankin Scale (mRS) scores 0–1 and 0–2, stroke recurrence and all-cause mortality. Secondary outcomes hemorrhagic transformation of infarction (HTI), Barthel Index, and NIHSS scores at multiple time points. Random-effects models were used to estimate pooled risk ratios (RR) or mean differences (MD) with 95% confidence intervals (CI) and heterogeneity was assessed with the I2 statistic.
Result:
From six studies, a total of 955 patients were included (remote ischemic conditioning [RIC] group: n = 502; sham/control group: n = 453). At 90 days, RIC was not associated with improved functional outcomes: mRS 0–1 (4 studies; RR 1.07, 95% CI 0.95–1.20; p = 0.26; I2 = 17%) or mRS 0–2 (4 studies; RR 1.03, 95% CI 0.89–1.03; p = 0.92; I2 = 64%). Stroke recurrence (4 studies; RR 1.04, 95% CI 0.67–1.59; p = 0.87; I2 = 0%), mortality (3 studies; RR 0.91, 95% CI 0.27–3.06; p = 0.87; I2 = 46%), HTI (3 studies; RR 1.12, 95% CI 0.59–2.11; p = 0.74; I2 = 0%), and Barthel Index (3 studies; MD 2.77, 95% CI –1.51 to 7.06; p = 0.20; I2 = 0%) showed no significant benefit with RIC. NIHSS scores were also comparable at 24 hours (2 studies; MD –0.28, 95% CI –0.84 to 0.27; p = 0.32), 7 days (3 studies; MD 0.01, 95% CI –0.49 to 0.50; p = 0.97), 30 days (2 studies; MD –0.63, 95% CI –1.38 to 0.12; p = 0.10), and last follow-up last follow-up (4 studies; MD –0.08, 95% CI –0.43 to 0.28; p = 0.67), all with I2 = 0%.
Conclusion:
This meta-analysis suggests patients with acute ischemic stroke treated with intravenous thrombolysis and remote ischemic conditioning (RIC) did not significantly improve functional outcomes, reduce stroke recurrence, mortality, or hemorrhagic transformation. No meaningful differences were observed in neurological recovery or activities of daily living.
More abstracts on this topic:
Age-related Differences in Peak Oxygen Uptake in Patients with Multimorbidity Undergoing Cardiac Rehabilitation
Gomes Pauline, Miller Sophie, Chacin-suarez Audry, Olson Thomas
Altered inflammatory state and mitochondrial function identified by transcriptomics in paediatric congenital heart patients prior to surgical repairBartoli-leonard Francesca, Harris Amy, Caputo Massimo