Final ID: Mo2037
Missed Opportunities for Cardiovascular Prevention in the United States: A Simulation-Based Analysis Using NHANES 2021–2022
Abstract Body (Do not enter title and authors here): Background
Despite clear guidelines, many high-risk individuals in the U.S. remain untreated for ASCVD prevention. We quantified the prevalence of missed treatment opportunities, identified sociodemographic predictors, and modeled long-term outcomes using a Markov framework.
Methods
We analyzed 9,215 adults aged ≥18 years from NHANES 2021–2022. Adults were eligible for preventive therapy if they had ASCVD, diabetes, cardiometabolic burden score ≥3, or were current smokers aged ≥40. Treatment was defined by use of any cardiovascular medication. A missed opportunity was defined as treatment-eligible but untreated. We used multivariable logistic regression to identify predictors and modeled ASCVD cases, deaths, QALYs, and costs over 5 years using a 3-state Markov model (Healthy, ASCVD, Death).
Results
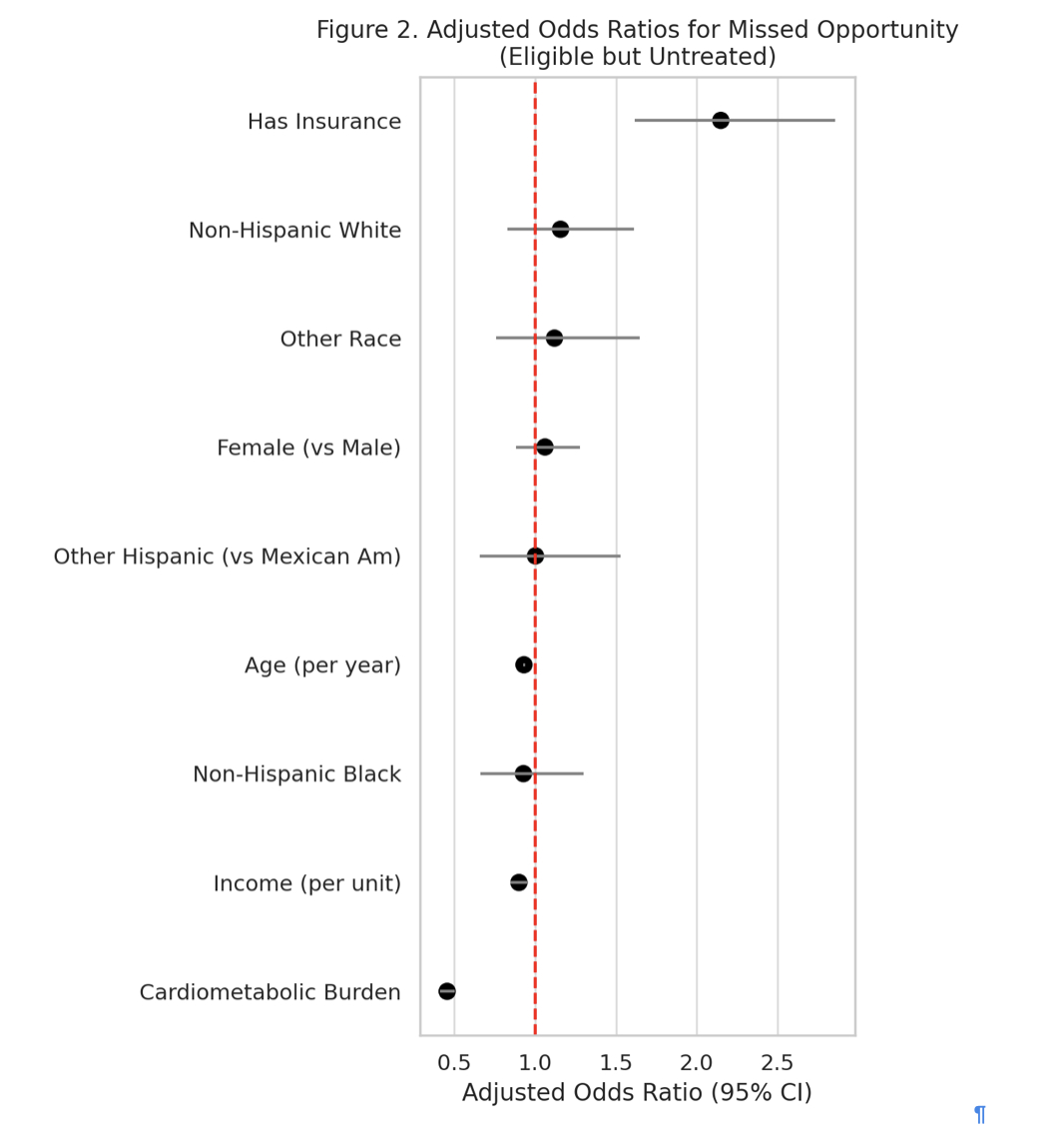
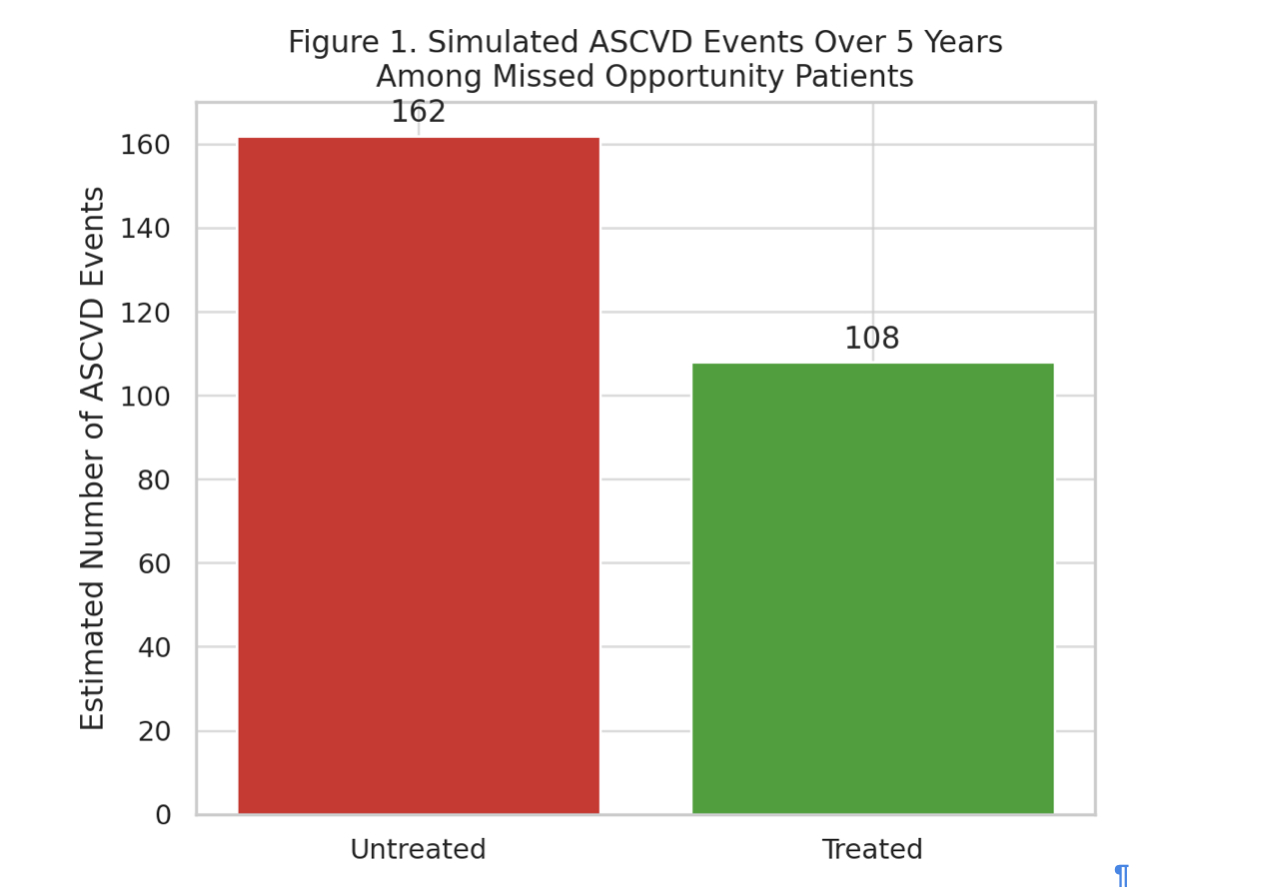
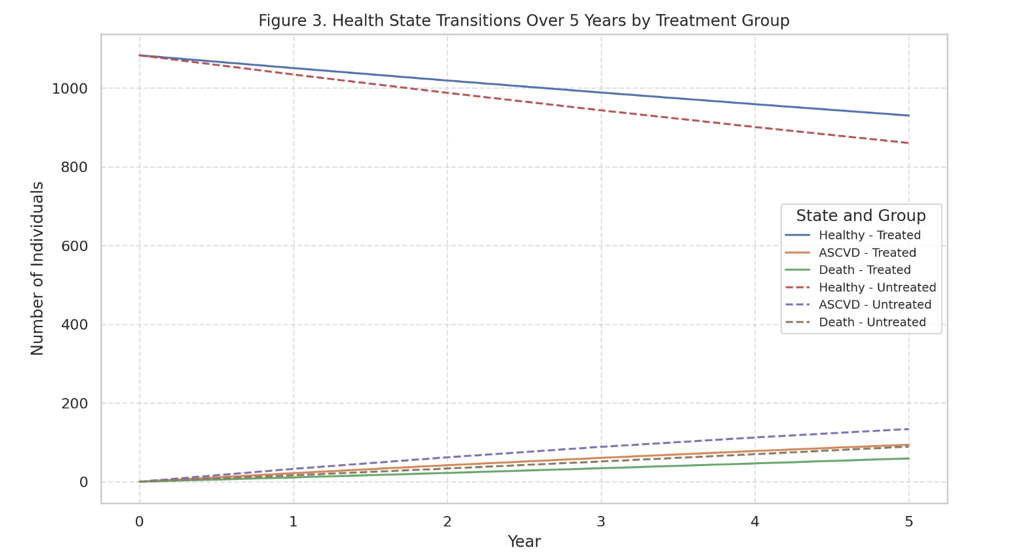
Of 2,756 eligible adults, 1,083 (39.3%) were not receiving any cardiovascular therapy. A missed opportunity was more likely among uninsured adults (OR 2.13, 95% CI: 1.61–2.84), those with income below the federal poverty line (OR 1.82, 95% CI: 1.31–2.52), and adults younger than 50 years (OR 1.94, 95% CI: 1.42–2.65) (Figure 1). Markov simulation projected 132 ASCVD cases and 88 deaths over 5 years in this untreated cohort, compared to 93 ASCVD cases and 60 deaths with preventive therapy (Figure 2). As shown in Figure 3, treatment preserved more individuals in the healthy state and slowed progression to ASCVD and death. Overall, preventive therapy resulted in 114 QALYs gained and $954,000 in cost savings per 1,083 adults over 5 years . When extrapolated nationally, over 1 million ASCVD events and $20 billion in costs could be prevented within 5 years.
Conclusions:
More than one-third of eligible U.S. adults are not receiving ASCVD preventive therapy. These missed opportunities represent not only lost years of life but also substantial cost and equity gaps that can be addressed through policy and population-level interventions.
Despite clear guidelines, many high-risk individuals in the U.S. remain untreated for ASCVD prevention. We quantified the prevalence of missed treatment opportunities, identified sociodemographic predictors, and modeled long-term outcomes using a Markov framework.
Methods
We analyzed 9,215 adults aged ≥18 years from NHANES 2021–2022. Adults were eligible for preventive therapy if they had ASCVD, diabetes, cardiometabolic burden score ≥3, or were current smokers aged ≥40. Treatment was defined by use of any cardiovascular medication. A missed opportunity was defined as treatment-eligible but untreated. We used multivariable logistic regression to identify predictors and modeled ASCVD cases, deaths, QALYs, and costs over 5 years using a 3-state Markov model (Healthy, ASCVD, Death).
Results
Of 2,756 eligible adults, 1,083 (39.3%) were not receiving any cardiovascular therapy. A missed opportunity was more likely among uninsured adults (OR 2.13, 95% CI: 1.61–2.84), those with income below the federal poverty line (OR 1.82, 95% CI: 1.31–2.52), and adults younger than 50 years (OR 1.94, 95% CI: 1.42–2.65) (Figure 1). Markov simulation projected 132 ASCVD cases and 88 deaths over 5 years in this untreated cohort, compared to 93 ASCVD cases and 60 deaths with preventive therapy (Figure 2). As shown in Figure 3, treatment preserved more individuals in the healthy state and slowed progression to ASCVD and death. Overall, preventive therapy resulted in 114 QALYs gained and $954,000 in cost savings per 1,083 adults over 5 years . When extrapolated nationally, over 1 million ASCVD events and $20 billion in costs could be prevented within 5 years.
Conclusions:
More than one-third of eligible U.S. adults are not receiving ASCVD preventive therapy. These missed opportunities represent not only lost years of life but also substantial cost and equity gaps that can be addressed through policy and population-level interventions.
More abstracts on this topic:
A Blood(y) Pressure Crisis: Diffuse Alveolar Hemorrhage as a Rare Manifestation of Severely Uncontrolled Hypertension
Nandyal Shreyas, Amdetsion Gedion Yilma, Varma Revati, Kohli Saksham, Hammo Hasan
A multifaceted family intervention for blood pressure management in rural China: an open label, parallel group, cluster randomized trial (Healthy Family Program)Jiang Chao, Dong Jianzeng, Cai Jun, Anderson Craig, Du Xin, Tang Yangyang, Han Rong, Song Yanna, Wang Chi, Lin Xiaolei, Yi Yang, Rodgers Anthony, Ma Changsheng