Final ID: MP236
Community Paramedic Home Visits for Heart Failure: Per-Protocol Analysis of the MIGHTy-Heart Trial
Abstract Body (Do not enter title and authors here): Background: Mobile Integrated Health (MIH) programs integrate nurse care coordination, community paramedic (CP) home visits, and telehealth visits with emergency medicine physicians. The MIGHTy-Heart pragmatic, randomized, controlled trial compared MIH to a transitions of care coordinator (TOCC), a nurse-led call 48–72 hours after discharge, among heart failure patients in 11 hospitals. In the trial, some patients randomized to MIH received a CP home visit while others did not, depending on clinical acuity and patient preference. This per-protocol analysis of the MIGHTy-Heart trial compares outcomes among patients randomized to MIH who received a CP home visit to patients randomized to TOCC.
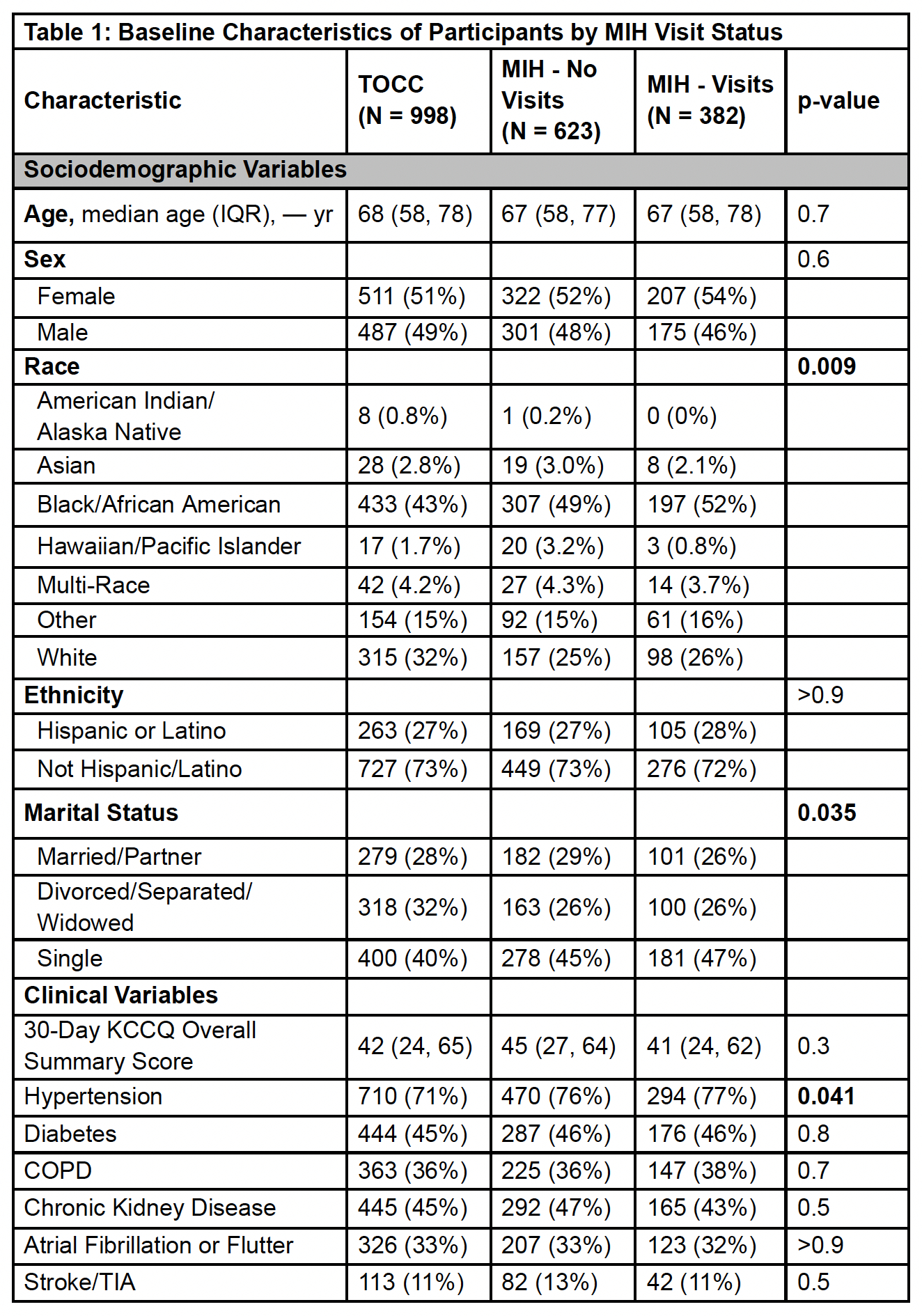
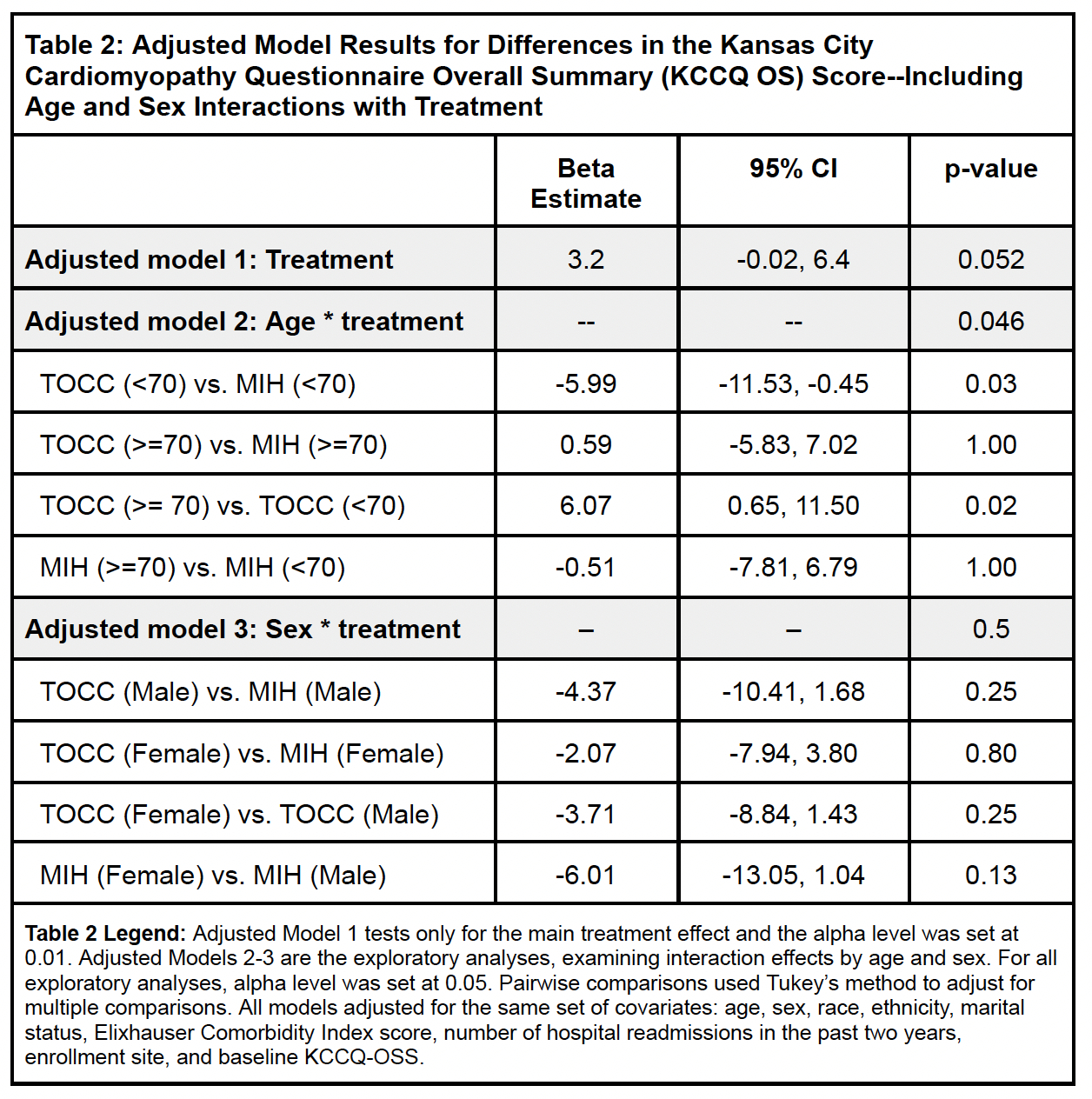
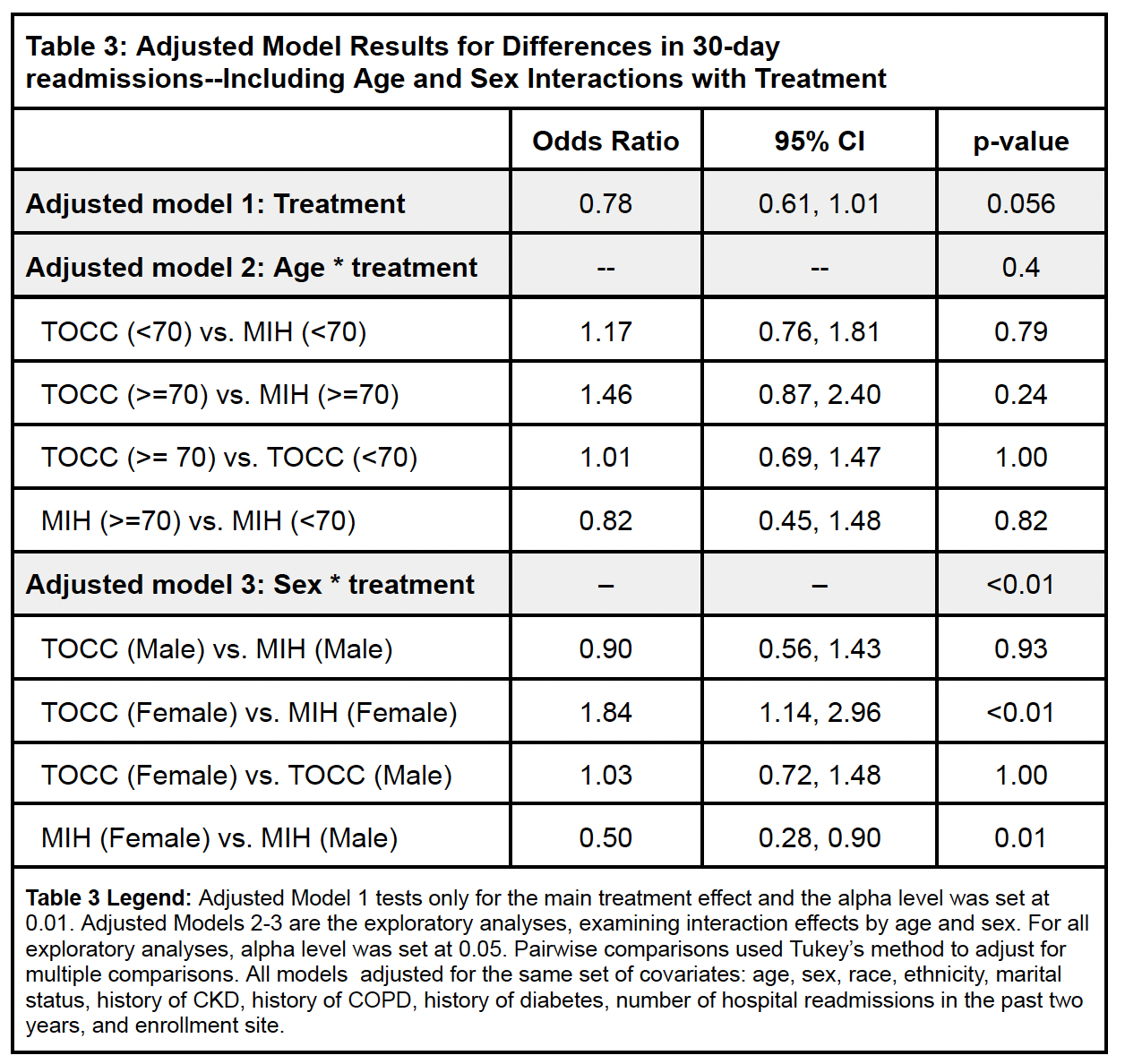
Methods: Of the 2003 patients enrolled, 998 were randomized to the TOCC arm and 1,005 to MIH, of which 382 (38%) received a CP home visit and did not crossover. Analyses compared MIH patients receiving a CP home visit (n=382) to TOCC (n=998). The co-primary outcomes were 30-day all-cause readmissions and change in health status measured using the Kansas City Cardiomyopathy Questionnaire (KCCQ). Weighted logistic regression models examining readmissions adjusted for age, sex, race, marital status, comorbidity burden, previous hospital readmissions, and enrollment site. Multivariable linear regression models examining health status adjusted for the same covariates, plus baseline KCCQ score. In exploratory analyses, we tested treatment-by-age and treatment-by-sex interactions for each outcome.
Results: The 2,003 patients’ mean age was 67.6 (standard deviation 13.7) years, 52% were female, 47% identified as Black or African American, and 27% as Hispanic. Few demographic differences existed between the arms (Table 1). In adjusted models, examining the interaction effect of sex and treatment on 30-day all-cause readmission, female MIH patients had 50% fewer odds of being readmitted compared to male MIH patients (p=0.01) (Table 2). In adjusted models, examining the interaction effect of age and treatment on 30-day health status, younger MIH patients scored, on average, 5.99 points higher than younger TOCC patients (p=0.03) (Table 3).
Conclusions: Compared to patients in the TOCC arm, women and younger patients in the MIH arm who received a CP home visit had reduced readmissions and improved health status, respectively. These findings align with the intention-to-treat analyses (reported separately) and support tailoring MIH services to the patients most likely to benefit.
Methods: Of the 2003 patients enrolled, 998 were randomized to the TOCC arm and 1,005 to MIH, of which 382 (38%) received a CP home visit and did not crossover. Analyses compared MIH patients receiving a CP home visit (n=382) to TOCC (n=998). The co-primary outcomes were 30-day all-cause readmissions and change in health status measured using the Kansas City Cardiomyopathy Questionnaire (KCCQ). Weighted logistic regression models examining readmissions adjusted for age, sex, race, marital status, comorbidity burden, previous hospital readmissions, and enrollment site. Multivariable linear regression models examining health status adjusted for the same covariates, plus baseline KCCQ score. In exploratory analyses, we tested treatment-by-age and treatment-by-sex interactions for each outcome.
Results: The 2,003 patients’ mean age was 67.6 (standard deviation 13.7) years, 52% were female, 47% identified as Black or African American, and 27% as Hispanic. Few demographic differences existed between the arms (Table 1). In adjusted models, examining the interaction effect of sex and treatment on 30-day all-cause readmission, female MIH patients had 50% fewer odds of being readmitted compared to male MIH patients (p=0.01) (Table 2). In adjusted models, examining the interaction effect of age and treatment on 30-day health status, younger MIH patients scored, on average, 5.99 points higher than younger TOCC patients (p=0.03) (Table 3).
Conclusions: Compared to patients in the TOCC arm, women and younger patients in the MIH arm who received a CP home visit had reduced readmissions and improved health status, respectively. These findings align with the intention-to-treat analyses (reported separately) and support tailoring MIH services to the patients most likely to benefit.
More abstracts on this topic:
A Case Presentation of Severe Left Ventricular Dysfunction from Focal Myocarditis due to Immune Checkpoint Inhibitor
Patel Romil, Hussain Kifah, Gordon Robert
5-oxoproline/ OPLAH Axis Alleviates Doxorubicin-induced Cardiomyopathy By Inhibiting FerroptosisJiang Meng, Guo Xinning