Final ID: MP57
Sedation Strategies in Cardiogenic Shock: Is Propofol Safer Than We Think?
Abstract Body (Do not enter title and authors here): Introduction:
Propofol has shown favorable outcomes in mechanically ventilated ICU patients, including shorter ventilation times, faster arousal, and reduced ICU stays. Despite these advantages, it is often avoided in cardiogenic shock due to concerns about hypotension and negative inotropic effects. However, there is limited evidence guiding sedative selection in this population. This study examines whether propofol use, compared to dexmedetomidine, fentanyl, and midazolam, is independently associated with differences in vasopressor requirements and in-hospital mortality among patients with cardiogenic shock.
Research Question:
Among CICU patients with cardiogenic shock, is propofol use independently associated with vasoactive-inotropic score (VIS) or in-hospital mortality compared to other commonly used sedatives?
Methods:
We conducted a retrospective cohort study of 3,480 adults admitted to the Northwell Health CICU (2016–2022) with a diagnosis of cardiogenic shock. Patients were grouped by predominant sedative exposure: propofol (reference), dexmedetomidine, fentanyl, midazolam, or mixed (no agent ≥75% of cumulative sedation shifts). Multivariable linear regression assessed the association between sedative group and VIS; logistic regression assessed in-hospital mortality. Models were adjusted for age, sex, Charlson Comorbidity Index, MAP, lactate, and creatinine.
Results/Data:
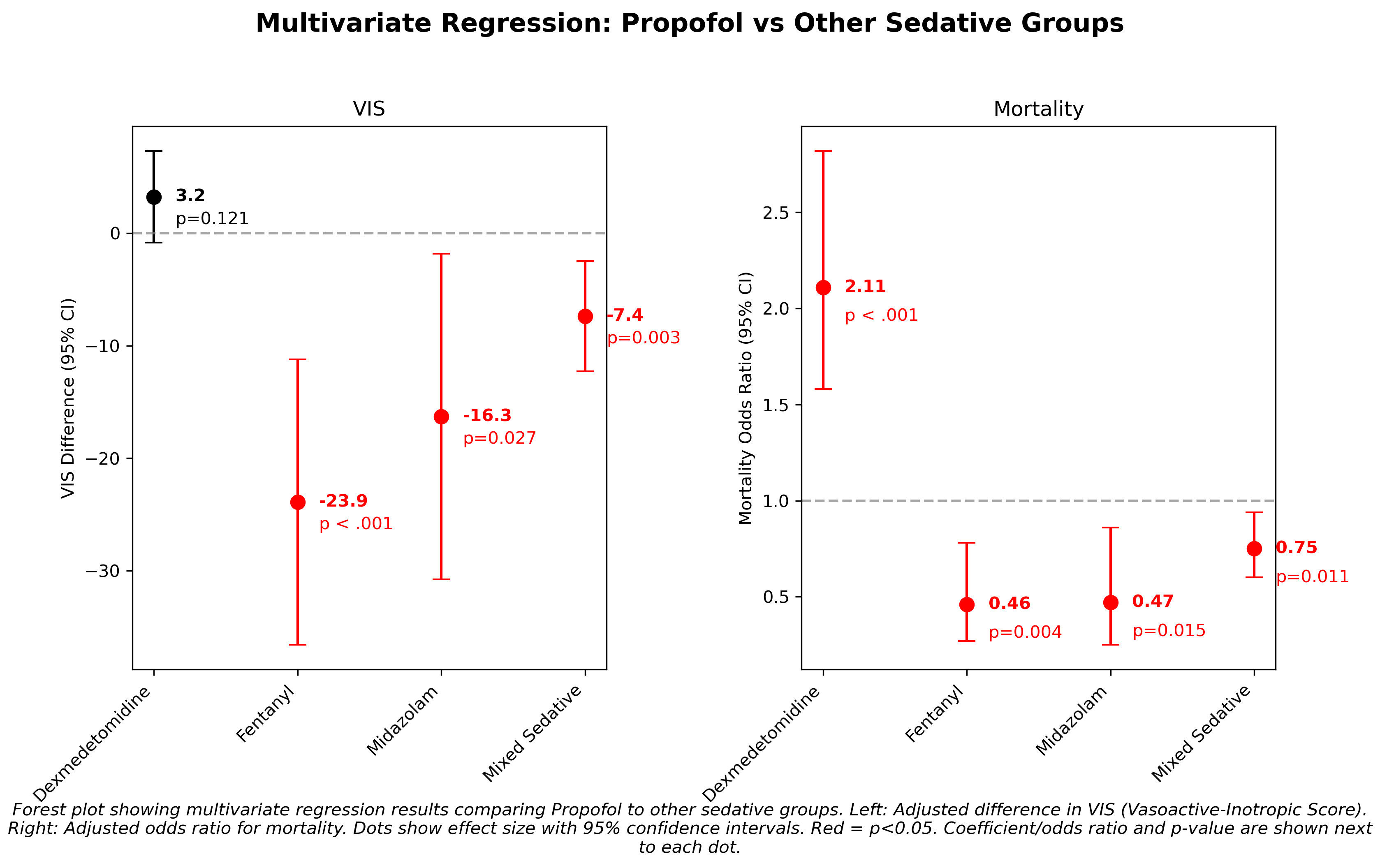
Compared to dexmedetomidine, propofol was associated with a higher VIS (β = +3.23, 95% CI: –0.85 to +7.31; p = 0.12), though not statistically significant. Propofol was associated with lower VIS compared to fentanyl (β = –23.89, p < 0.001), midazolam (β = –16.29, p = 0.027), and mixed sedatives (β = –7.39, p = 0.003). Propofol use was associated with higher odds of mortality versus dexmedetomidine (OR = 2.11, p < 0.001), but lower odds versus fentanyl (OR = 0.46, p = 0.004), midazolam (OR = 0.47, p = 0.016), and mixed sedatives (OR = 0.75, p = 0.011).
Conclusion:
After adjusting for clinical and hemodynamic variables, propofol use was independently associated with lower vasopressor/inotrope requirements and reduced mortality compared to fentanyl, midazolam, and mixed sedatives. The higher mortality compared to dexmedetomidine may reflect selection bias, as it is often used in less critically ill patients requiring lighter sedation. These findings support continued use of propofol in cardiogenic shock when appropriate, though prospective studies are needed to confirm causality.
Propofol has shown favorable outcomes in mechanically ventilated ICU patients, including shorter ventilation times, faster arousal, and reduced ICU stays. Despite these advantages, it is often avoided in cardiogenic shock due to concerns about hypotension and negative inotropic effects. However, there is limited evidence guiding sedative selection in this population. This study examines whether propofol use, compared to dexmedetomidine, fentanyl, and midazolam, is independently associated with differences in vasopressor requirements and in-hospital mortality among patients with cardiogenic shock.
Research Question:
Among CICU patients with cardiogenic shock, is propofol use independently associated with vasoactive-inotropic score (VIS) or in-hospital mortality compared to other commonly used sedatives?
Methods:
We conducted a retrospective cohort study of 3,480 adults admitted to the Northwell Health CICU (2016–2022) with a diagnosis of cardiogenic shock. Patients were grouped by predominant sedative exposure: propofol (reference), dexmedetomidine, fentanyl, midazolam, or mixed (no agent ≥75% of cumulative sedation shifts). Multivariable linear regression assessed the association between sedative group and VIS; logistic regression assessed in-hospital mortality. Models were adjusted for age, sex, Charlson Comorbidity Index, MAP, lactate, and creatinine.
Results/Data:
Compared to dexmedetomidine, propofol was associated with a higher VIS (β = +3.23, 95% CI: –0.85 to +7.31; p = 0.12), though not statistically significant. Propofol was associated with lower VIS compared to fentanyl (β = –23.89, p < 0.001), midazolam (β = –16.29, p = 0.027), and mixed sedatives (β = –7.39, p = 0.003). Propofol use was associated with higher odds of mortality versus dexmedetomidine (OR = 2.11, p < 0.001), but lower odds versus fentanyl (OR = 0.46, p = 0.004), midazolam (OR = 0.47, p = 0.016), and mixed sedatives (OR = 0.75, p = 0.011).
Conclusion:
After adjusting for clinical and hemodynamic variables, propofol use was independently associated with lower vasopressor/inotrope requirements and reduced mortality compared to fentanyl, midazolam, and mixed sedatives. The higher mortality compared to dexmedetomidine may reflect selection bias, as it is often used in less critically ill patients requiring lighter sedation. These findings support continued use of propofol in cardiogenic shock when appropriate, though prospective studies are needed to confirm causality.
More abstracts on this topic:
A Case of Concomitant Wild-Type Transthyretin and Systemic Light Chain Amyloidosis Involving Separate Organs
Chiu Leonard, Afrough Aimaz, Nadeem Urooba, Jebakumar Deborah, Grodin Justin
APOL1 Risk Variants in Preeclampsia: From Mechanistic Insights to Therapeutic OpportunitiesRao Vivikta, Waikar Sushrut, Wei Jin, Fu Jiayi, Liaw Easton, De Thea, Sedarski Jonathan, Tang Janice, Zhang Jie, Kuohung Wendy, Ilori Titilayo