Final ID: MP621
Rural–Urban Disparities in Cardiac Disease Outcomes: An EHR-Based Cohort Study in Missouri
Abstract Body (Do not enter title and authors here): Background
Cardiovascular disease remains the leading cause of death in the U.S., and rural residents have more difficult access to the same medical care that urban residents have. Using a population study approach, we compared rural versus urban cardiac patients’ survival, healthcare use, and social risk factors in Missouri.
Methods
We performed a retrospective cohort study of adults diagnosed with ischemic heart disease, heart failure, arrhythmias, cerebrovascular disease, and related conditions (ICD-10 codes) between January 2016 and December 2024. Data (PCORnet CDM) included demographics, rural/urban status (RUCA), clinical risks (hyperlipidemia, diabetes, BMI, obesity, smoking), and social determinants (employment insecurity, housing instability, psychosocial concerns, insurance, DNR status). Baseline comparisons used chi-square or Wilcoxon tests. Two-year post-diagnosis utilization (office visits, ED visits, length of stay) was modeled via Poisson regression. Survival was assessed with Kaplan-Meier curves and Cox models, first unadjusted (rural vs. urban) then adjusted for age, sex, and BMI. Schoenfeld residuals tested proportional hazards.
Results
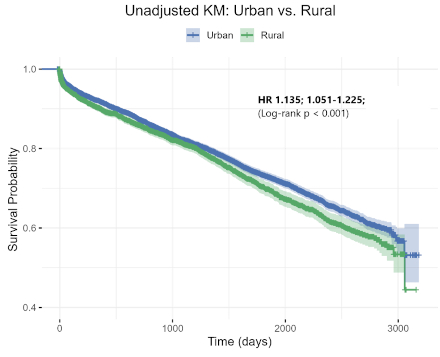
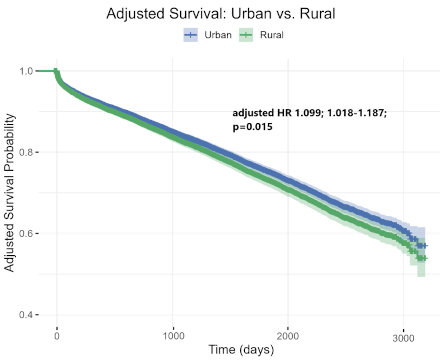
Among 23,349 patients (9,280 rural; 14,069 urban), rural patients were more often White (87.8% vs. 76.1%) and had higher social risk: employment insecurity (2.2% vs. 1.2%) and housing instability (5.3% vs. 3.2%). Obesity (62%) and smoking (20%) were similar. Two years post-diagnosis, rural patients had 21.3% fewer outpatient visits (IRR 0.787; 95% CI 0.762-0.813), with similar ED use and shorter stays. Unadjusted survival was lower for rural patients (log-rank p < 0.001). Unadjusted Cox showed rural status confers 13.5% higher hazard (HR 1.135; 1.051-1.225; p = 0.001). After adjusting for age (HR 1.048 per year; p < 0.001), male sex (HR 1.180; p < 0.001), and BMI (HR 0.996 per unit; p=0.045), rural residence remained an independent predictor (adjusted HR 1.099; 1.018-1.187; p=0.015).
Conclusions
Rural cardiac patients have higher mortality than urban patients, even after accounting for age, sex, and BMI. They also face greater social risk and reduced outpatient access, likely worsening outcomes. Interventions should expand rural outpatient services, address social determinants (employment, housing), and strengthen rural health systems to deliver continuous, patient-centered cardiac care.
Cardiovascular disease remains the leading cause of death in the U.S., and rural residents have more difficult access to the same medical care that urban residents have. Using a population study approach, we compared rural versus urban cardiac patients’ survival, healthcare use, and social risk factors in Missouri.
Methods
We performed a retrospective cohort study of adults diagnosed with ischemic heart disease, heart failure, arrhythmias, cerebrovascular disease, and related conditions (ICD-10 codes) between January 2016 and December 2024. Data (PCORnet CDM) included demographics, rural/urban status (RUCA), clinical risks (hyperlipidemia, diabetes, BMI, obesity, smoking), and social determinants (employment insecurity, housing instability, psychosocial concerns, insurance, DNR status). Baseline comparisons used chi-square or Wilcoxon tests. Two-year post-diagnosis utilization (office visits, ED visits, length of stay) was modeled via Poisson regression. Survival was assessed with Kaplan-Meier curves and Cox models, first unadjusted (rural vs. urban) then adjusted for age, sex, and BMI. Schoenfeld residuals tested proportional hazards.
Results
Among 23,349 patients (9,280 rural; 14,069 urban), rural patients were more often White (87.8% vs. 76.1%) and had higher social risk: employment insecurity (2.2% vs. 1.2%) and housing instability (5.3% vs. 3.2%). Obesity (62%) and smoking (20%) were similar. Two years post-diagnosis, rural patients had 21.3% fewer outpatient visits (IRR 0.787; 95% CI 0.762-0.813), with similar ED use and shorter stays. Unadjusted survival was lower for rural patients (log-rank p < 0.001). Unadjusted Cox showed rural status confers 13.5% higher hazard (HR 1.135; 1.051-1.225; p = 0.001). After adjusting for age (HR 1.048 per year; p < 0.001), male sex (HR 1.180; p < 0.001), and BMI (HR 0.996 per unit; p=0.045), rural residence remained an independent predictor (adjusted HR 1.099; 1.018-1.187; p=0.015).
Conclusions
Rural cardiac patients have higher mortality than urban patients, even after accounting for age, sex, and BMI. They also face greater social risk and reduced outpatient access, likely worsening outcomes. Interventions should expand rural outpatient services, address social determinants (employment, housing), and strengthen rural health systems to deliver continuous, patient-centered cardiac care.
More abstracts on this topic:
Association Between Rurality and Socioeconomic Status on Acute Myocardial Infarction Hospitalization Among Medicare Beneficiaries
Quadri Fayz, Dalmacy Djhenne, Kanneganti Nitin, Rabah Abdullah, Berry Jarett, Tiruneh Yordanos
25-Year Decline in Aortic Aneurysm and Dissection Mortality in the U.S.: Impact of Endovascular Repair and Forecast to 2030Ali Manzer, Umar Haddaya, Nazir Tahira, Nizam Muhammad, Steafo Lark, Sharif Ayesha, Jehangir Hanzala, Arham Muhammad, Hamza Anfal, Hassan Arbaz, Amjad Ans, Ali Iman, Zuha Zuha