Final ID: MP2522
A Remote Patient Care Heart Failure Program Drives Improved Clinical Outcomes and Reduced Healthcare Cost and Utilization
Abstract Body (Do not enter title and authors here): Introduction
Despite significant support of the clinical benefits of GDMT, heart failure (HF) patients have poor clinical outcomes and as a result high healthcare costs and utilization.
Hypothesis
A remote patient care (RPC) program led by a team of clinicians can drive improved clinical outcomes and reduced healthcare costs and utilization for HF patients at scale.
Methods
Medicare patients with HF (EHR-based ICD-10 codes) across 19 states were enrolled into a RPC program from Aug 2021 to Feb 2024. The program integrates home-based BP, HR, weights, patient-reported symptoms, and clinical guidelines into a technology-enabled, proactive care model to facilitate vitals, symptoms and GDMT optimization. A retrospective difference-in-difference analysis of Medicare claims data was conducted to evaluate the RPC program’s impact on healthcare costs and utilization over 12 months following activation, comparing enrolled patients to a propensity score-matched control group in the VRDC.
Results
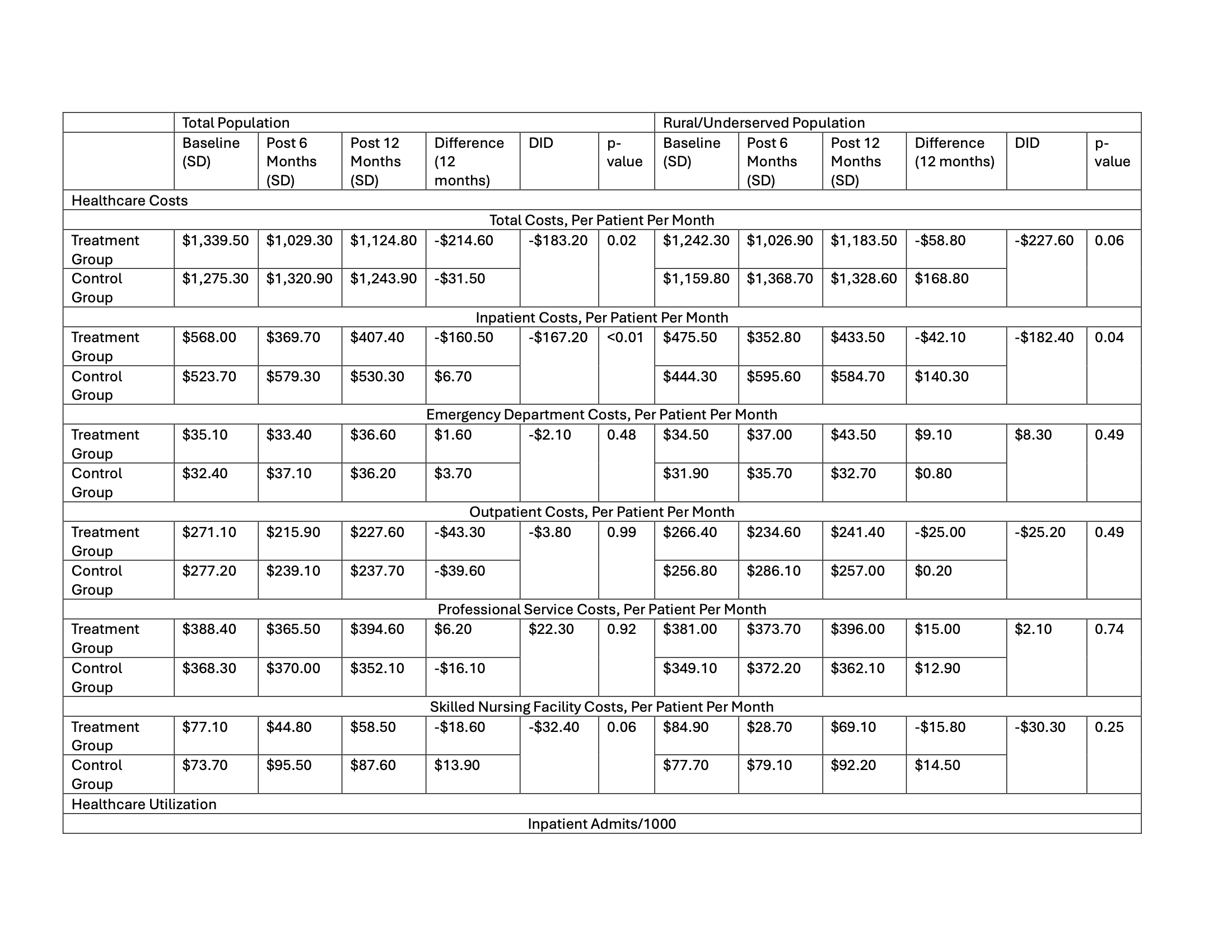
The outcomes analysis included 2,697 enrolled patients (mean(SD) age: 75(10)years, BP 136/78(18/10)mmHg, weight 197(53)lbs; female: 49%, white: 50%, rural/underserved: 55%) followed for a mean (SD) of 58(29) weeks. HFrEF (mean (SD) EF 35(10)%) and HFpEF (mean (SD) EF 60(7)%) was present in 42% and 58% patients, respectively. There was a statistically significant decrease in BP (-7/4mmHg) and weight (-5lbs) [p<0.001], but not HR. Among HFrEF patients, ~3 times more patients were prescribed all four pillars of GDMT at follow-up compared to baseline (26.9% vs. 9.8%, p<0.001), with significant improvements in the percentage of patients prescribed >50% target dose for each GDMT pillar. Among HFpEF patients, ~2 times more patients were on a SGLT2i (35.3% vs. 17.6%, p<0.001) and MRA (29.6% vs. 15.9%, p<0.001) at follow-up compared to baseline. The cost and utilization analysis included 1,786 enrolled and 3,401 control Medicare FFS patients who were followed for an average of 10(2) months. The RPC program resulted in a significant reduction in total cost of care (-$183 PMPM; p<0.05) over 12 months, driven primarily by a reduction in inpatient costs (-$167 PMPM, p<0.001) and admissions (-77 vs. 0/1000, 18% reduction; p<0.05). Clinical, costs and utilization results were similar among patients living in rural/underserved areas.
Conclusions
A nationwide RPC HF program improves use and dose of GDMT while also reducing healthcare costs and utilization for HF patients across the US.
Despite significant support of the clinical benefits of GDMT, heart failure (HF) patients have poor clinical outcomes and as a result high healthcare costs and utilization.
Hypothesis
A remote patient care (RPC) program led by a team of clinicians can drive improved clinical outcomes and reduced healthcare costs and utilization for HF patients at scale.
Methods
Medicare patients with HF (EHR-based ICD-10 codes) across 19 states were enrolled into a RPC program from Aug 2021 to Feb 2024. The program integrates home-based BP, HR, weights, patient-reported symptoms, and clinical guidelines into a technology-enabled, proactive care model to facilitate vitals, symptoms and GDMT optimization. A retrospective difference-in-difference analysis of Medicare claims data was conducted to evaluate the RPC program’s impact on healthcare costs and utilization over 12 months following activation, comparing enrolled patients to a propensity score-matched control group in the VRDC.
Results
The outcomes analysis included 2,697 enrolled patients (mean(SD) age: 75(10)years, BP 136/78(18/10)mmHg, weight 197(53)lbs; female: 49%, white: 50%, rural/underserved: 55%) followed for a mean (SD) of 58(29) weeks. HFrEF (mean (SD) EF 35(10)%) and HFpEF (mean (SD) EF 60(7)%) was present in 42% and 58% patients, respectively. There was a statistically significant decrease in BP (-7/4mmHg) and weight (-5lbs) [p<0.001], but not HR. Among HFrEF patients, ~3 times more patients were prescribed all four pillars of GDMT at follow-up compared to baseline (26.9% vs. 9.8%, p<0.001), with significant improvements in the percentage of patients prescribed >50% target dose for each GDMT pillar. Among HFpEF patients, ~2 times more patients were on a SGLT2i (35.3% vs. 17.6%, p<0.001) and MRA (29.6% vs. 15.9%, p<0.001) at follow-up compared to baseline. The cost and utilization analysis included 1,786 enrolled and 3,401 control Medicare FFS patients who were followed for an average of 10(2) months. The RPC program resulted in a significant reduction in total cost of care (-$183 PMPM; p<0.05) over 12 months, driven primarily by a reduction in inpatient costs (-$167 PMPM, p<0.001) and admissions (-77 vs. 0/1000, 18% reduction; p<0.05). Clinical, costs and utilization results were similar among patients living in rural/underserved areas.
Conclusions
A nationwide RPC HF program improves use and dose of GDMT while also reducing healthcare costs and utilization for HF patients across the US.
More abstracts on this topic:
Americans’ Views on Healthcare Coverage, Access, and Equity in the US: Implications for Cardiovascular Health
Perera Sudheesha, Wadhera Rishi, Khullar Dhruv
A Community Outreach Program Focused on Hypertension Awareness Reaches 600+ People in Rural Georgia and Works to Build the Next Generation of Biomedical ScientistsDent Elena, Ilatovskaya Daria, Pinkerton Brittany, Crider Emily, Ryan Michael, Sullivan Jennifer