Final ID: MP820
Long-Term Impact of GLP-1 Receptor Agonists on Cardiovascular Outcomes in Patients Treated with Hematopoietic Stem Cell Transplantation: A Propensity-Score Matched Analysis
Abstract Body (Do not enter title and authors here): Background: Effective risk factor modification, including management of obesity and diabetes mellitus (DM), is essential to mitigating cardiovascular complications after hematopoietic stem cell transplantation (HSCT). Given the growing use of GLP-1 receptor agonists (GLP-1 RAs), large-scale studies are needed to assess their cardiovascular impact in patients undergoing HSCT.
Methods: Using the TriNetX network, we identified patients who underwent HSCT and had DM or obesity. Patients were categorized into two cohorts: those who received GLP-1 RAs and those who did not. Outcomes, including all-cause mortality, all-cause hospitalization, acute myocardial infarction (AMI), atrial fibrillation (AF), cerebrovascular accident (CVA), and heart failure (HF) exacerbation, were assessed at 1 year, 3 years, and 5 years follow-up. Cohorts were propensity score-matched based on medical comorbidities, transplant diagnoses, and conditioning regimens.
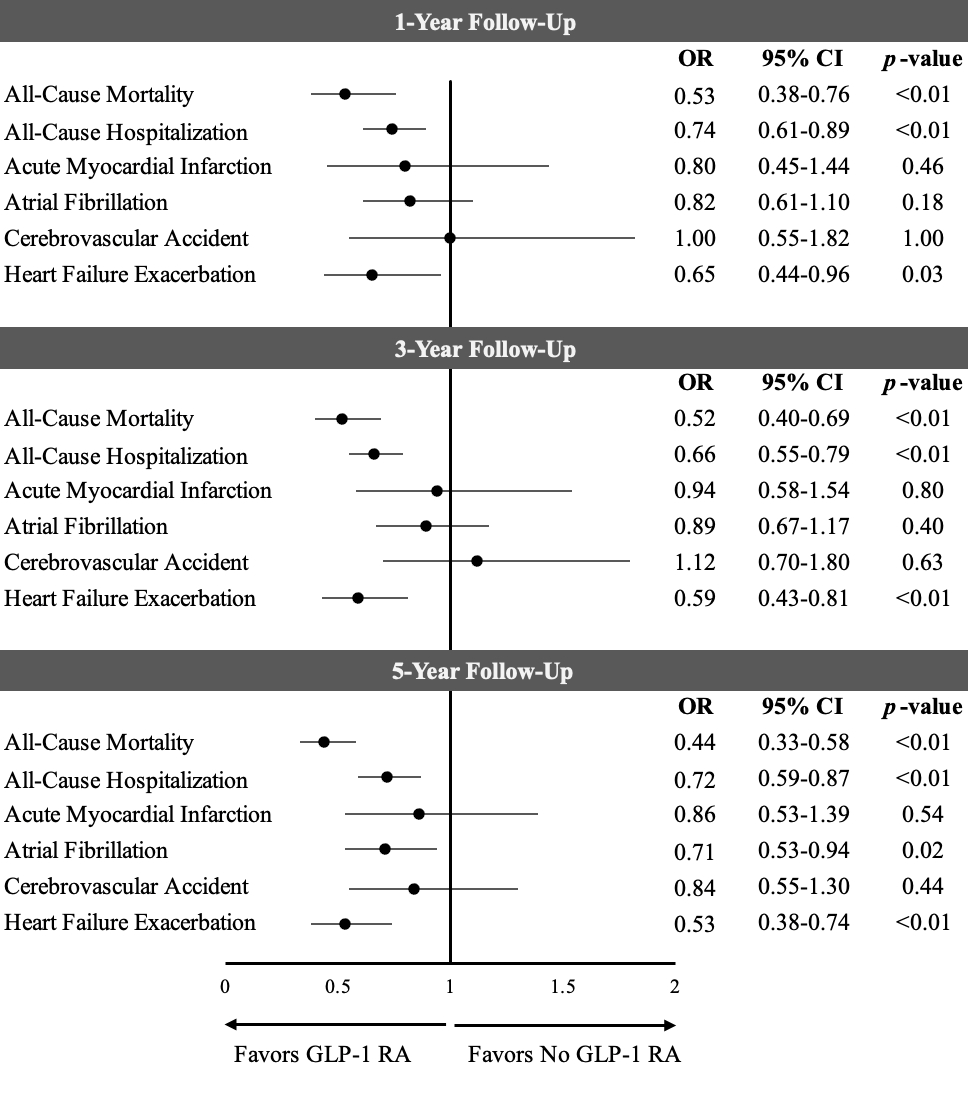
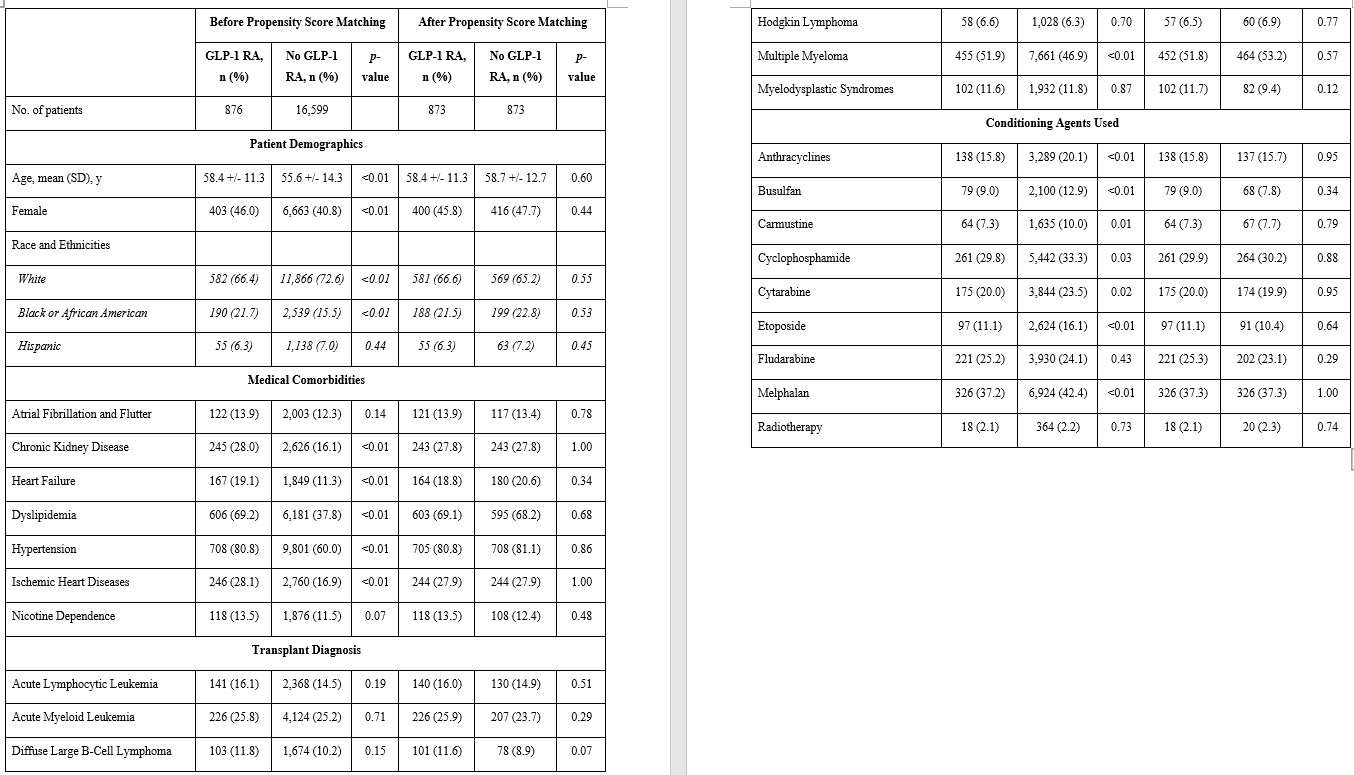
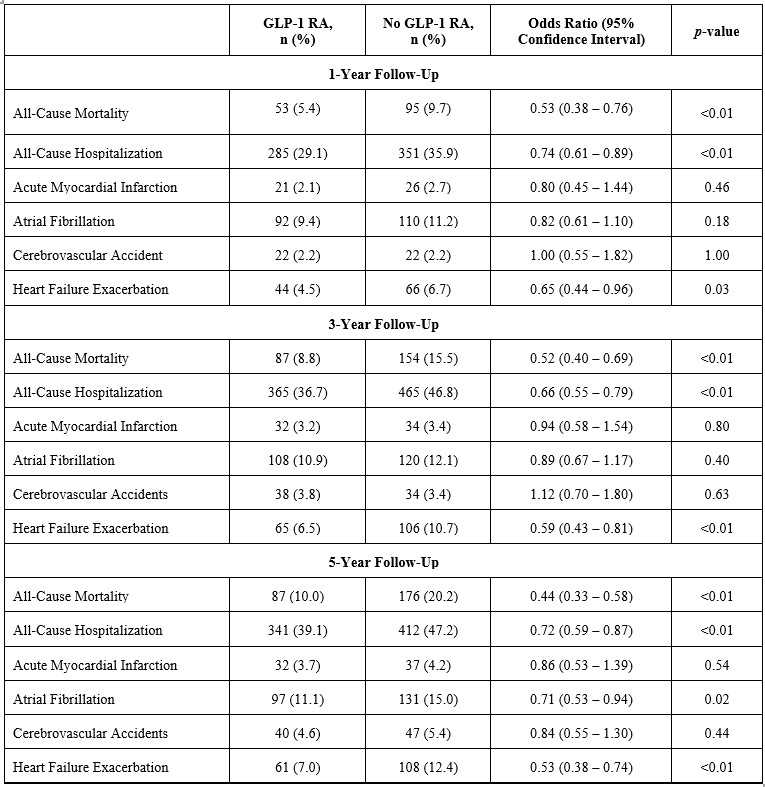
Results: Of the initial 17,475 patients with HSCT and DM/obesity, 876 (5.0%, 46.0% females, mean age 58.4 +/- 11.3 years old) received GLP-1 RA and 16,599 (95.0%, 40.8% females, mean age 55.6 +/- 14.3 years old) did not. After propensity score matching, 873 patients were divided equally into each cohort (Table). GLP-1 RA was associated with lower odds of all-cause mortality (1-year: odds ratio [OR]: 0.53; 95% confidence interval [CI]: 0.38–0.76; p<0.01; 3-year: OR: 0.52; CI: 0.40–0.69; p<0.01; 5-year: OR: 0.44; CI: 0.33–0.58; p<0.01), all-cause hospitalization (1-year: OR: 0.74; CI: 0.61–0.89; p<0.01; 3-year: OR: 0.66; CI: 0.55–0.79; p<0.01; 5-year: OR: 0.72; CI: 0.59–0.87; p<0.01), and HF exacerbation (1-year: OR: 0.65; CI: 0.44–0.96; p=0.03; 3-year: OR: 0.59; CI: 0.43–0.81; p<0.01; 5-year: OR: 0.53; CI: 0.38–0.74; p<0.01), compared to the non–GLP-1 RA group. At 5-year follow-up, GLP-1 RA use was also associated with lower odds of AF (OR: 0.71; CI: 0.53–0.94; p=0.02). No significant differences were noted in AMI or CVA at 1-, 3-, and 5-years of follow-up.
Conclusion: After propensity score-matching in this retrospective cohort study, GLP-1 RA use was associated with significantly lower odds of all-cause mortality, all-cause hospitalization, and heart failure exacerbation at 1-, 3-, and 5-year of follow-up in patients with DM/obesity who underwent HSCT. At 5 years, use of GLP-1 RA was associated with lower odds of AF.
Methods: Using the TriNetX network, we identified patients who underwent HSCT and had DM or obesity. Patients were categorized into two cohorts: those who received GLP-1 RAs and those who did not. Outcomes, including all-cause mortality, all-cause hospitalization, acute myocardial infarction (AMI), atrial fibrillation (AF), cerebrovascular accident (CVA), and heart failure (HF) exacerbation, were assessed at 1 year, 3 years, and 5 years follow-up. Cohorts were propensity score-matched based on medical comorbidities, transplant diagnoses, and conditioning regimens.
Results: Of the initial 17,475 patients with HSCT and DM/obesity, 876 (5.0%, 46.0% females, mean age 58.4 +/- 11.3 years old) received GLP-1 RA and 16,599 (95.0%, 40.8% females, mean age 55.6 +/- 14.3 years old) did not. After propensity score matching, 873 patients were divided equally into each cohort (Table). GLP-1 RA was associated with lower odds of all-cause mortality (1-year: odds ratio [OR]: 0.53; 95% confidence interval [CI]: 0.38–0.76; p<0.01; 3-year: OR: 0.52; CI: 0.40–0.69; p<0.01; 5-year: OR: 0.44; CI: 0.33–0.58; p<0.01), all-cause hospitalization (1-year: OR: 0.74; CI: 0.61–0.89; p<0.01; 3-year: OR: 0.66; CI: 0.55–0.79; p<0.01; 5-year: OR: 0.72; CI: 0.59–0.87; p<0.01), and HF exacerbation (1-year: OR: 0.65; CI: 0.44–0.96; p=0.03; 3-year: OR: 0.59; CI: 0.43–0.81; p<0.01; 5-year: OR: 0.53; CI: 0.38–0.74; p<0.01), compared to the non–GLP-1 RA group. At 5-year follow-up, GLP-1 RA use was also associated with lower odds of AF (OR: 0.71; CI: 0.53–0.94; p=0.02). No significant differences were noted in AMI or CVA at 1-, 3-, and 5-years of follow-up.
Conclusion: After propensity score-matching in this retrospective cohort study, GLP-1 RA use was associated with significantly lower odds of all-cause mortality, all-cause hospitalization, and heart failure exacerbation at 1-, 3-, and 5-year of follow-up in patients with DM/obesity who underwent HSCT. At 5 years, use of GLP-1 RA was associated with lower odds of AF.
More abstracts on this topic:
Aspirin for Primary Prevention of Cardiovascular Events in Patients with Diabetes Mellitus: An Updated Systematic Review, Meta-Analysis & Trial Sequential Analysis of Randomized Controlled Trials post-ASCEND Trial
Puthia Valappil Omer Mohammed, John M Rose, Mallikarjun Samanth, D Souza Leroy, Rongala Sai Anurag, Chakraborty Diya, Balarishnan Rojith, Kutty Shelby
Clinical scale MSC-derived extracellular vesicles enhance poststroke neuroplasticity in a non-human primate model of strokeBang Oh Young, Son Jeong Pyo, Kim Eun Hee, Chopp Michael