Final ID: MP812
Point-of-care Non-invasive Classification of Elevated Intracardiac Filling Pressures for Congestion Assessment
Abstract Body (Do not enter title and authors here): Background: Pulmonary capillary wedge pressure (PCWP) provides an objective assessment of congestion status in heart failure (HF) patients, but its use is limited by the need for an invasive procedure, trained personnel, and specialized equipment to obtain a measurement. Cardiosense (Chicago, IL) has developed a machine learning (ML) algorithm that detects elevated PCWP non-invasively from data acquired by a chest-worn wearable device (CardioTag). We present data for a potential in-clinic point-of-care tool that improves the identification of hemodynamic congestion, with a focus on outpatient and low-acuity settings.
Methods: The ePCWP System is a ML model developed to identify elevated PCWP (>18 mmHg) using non-invasive physiological biosignals from the CardioTag device, which simultaneously collects electrocardiogram, seismocardiogram, and photoplethysmogram data. Concurrent CardioTag and right-heart catheterization (RHC) data were collected prospectively in an observational study across 15 US sites from 1,116 patients undergoing standard-of-care RHC. Patients were either diagnosed with HFrEF, HFpEF, HFmrEF, or were suspected of HF before the RHC procedure. Standard of care physical examination, used to evaluate congestion status, was captured and used for comparative analysis. The training dataset contained 726 subjects and the validation dataset contained 153 subjects.
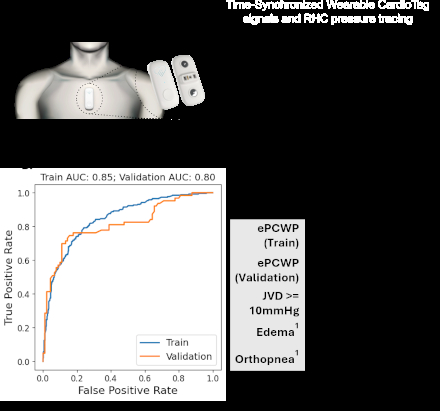
Results: Five-fold cross-validation of the training dataset showed an overall accuracy of 0.79, sensitivity of 0.75 (CI: [0.69, 0.80]), and a specificity of 0.81 (CI: [0.77, 0.85]). The validation dataset showed an overall accuracy of 0.81, sensitivity of 0.76 (CI: [0.63, 0.86]), and a specificity of 0.82 (CI: [0.72, 0.89]). Figure 1 shows the overall classification performance of the ePCWP System (left) and a comparison to standard-of-care physical exam (right).
Conclusion: We developed a non-invasive point-of-care tool that is capable of providing rapid, accurate assessments of congestion for patients with HF. This tool might be used to support convenient, frequent inpatient monitoring to augment discharge decisions and guide post-discharge follow-up care towards timely interventions and improvements in patient outcomes.
Methods: The ePCWP System is a ML model developed to identify elevated PCWP (>18 mmHg) using non-invasive physiological biosignals from the CardioTag device, which simultaneously collects electrocardiogram, seismocardiogram, and photoplethysmogram data. Concurrent CardioTag and right-heart catheterization (RHC) data were collected prospectively in an observational study across 15 US sites from 1,116 patients undergoing standard-of-care RHC. Patients were either diagnosed with HFrEF, HFpEF, HFmrEF, or were suspected of HF before the RHC procedure. Standard of care physical examination, used to evaluate congestion status, was captured and used for comparative analysis. The training dataset contained 726 subjects and the validation dataset contained 153 subjects.
Results: Five-fold cross-validation of the training dataset showed an overall accuracy of 0.79, sensitivity of 0.75 (CI: [0.69, 0.80]), and a specificity of 0.81 (CI: [0.77, 0.85]). The validation dataset showed an overall accuracy of 0.81, sensitivity of 0.76 (CI: [0.63, 0.86]), and a specificity of 0.82 (CI: [0.72, 0.89]). Figure 1 shows the overall classification performance of the ePCWP System (left) and a comparison to standard-of-care physical exam (right).
Conclusion: We developed a non-invasive point-of-care tool that is capable of providing rapid, accurate assessments of congestion for patients with HF. This tool might be used to support convenient, frequent inpatient monitoring to augment discharge decisions and guide post-discharge follow-up care towards timely interventions and improvements in patient outcomes.
More abstracts on this topic:
A Phase 2a randomized controlled trial of once-daily versus twice-daily remote ischemic conditioning in vascular cognitive impairment (TRIC-VCI)
Ganesh Aravind, Mccreary Cheryl, Sahlas Demetrios, Sharma Mukul, Swartz Richard, Smith Eric, Barber Philip, Black Sandra, Corbett Dale, Field Thalia, Frayne Richard, Hachinski Vladimir, Ismail Zahinoor, Mai Lauren
A rare case of ventriculobronchial fistula caused by an epicardial defibrillator patchAlampoondi Venkataramanan Sai Vikram, Windle John