Final ID: MP274
Impact of a Cardiogenic Shock Team Approach on Outcomes in a Non-LVAD Center
Abstract Body (Do not enter title and authors here): Introduction: Cardiogenic shock (CS) is a high-mortality clinical syndrome, with reported rates between 40–50%. Multidisciplinary shock teams have emerged to streamline care and improve outcomes. In our non-LVAD center, we implemented a structured shock team model involving interventional cardiology, advanced heart failure, and critical care physicians, with early decision-making led primarily by an interventional and transplant cardiologist. Standardized protocols guided management and mechanical circulatory support (MCS) selection.
Methods: We performed a retrospective review of adult patients with cardiogenic shock admitted between 2024–2025. Inclusion required ≥2 of the following: MAP <60 mmHg or a ≥30 mmHg drop from baseline, SBP <90 mmHg or ≥30 mmHg drop from baseline, HR >100 bpm, cardiac index less than 2.2 L per min per m2, PAPI <1.0, cardiac power output <0.6 W, or vasopressor/MCS requirement. Clinical, hemodynamic, and echocardiographic data were extracted from electronic records. The primary outcome was in-hospital mortality; secondary outcomes included MCS use, escalation timing, and transfer rate.
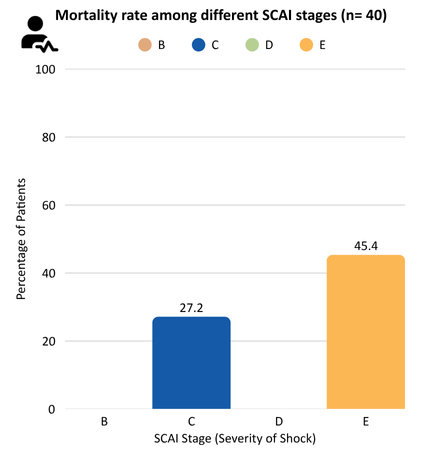
Results: A total of 40 patients were included (mean age 59.3 ± 13.6 years). The leading etiology was acute decompensated heart failure (51.2%), followed by NSTEMI (20.9%) and STEMI (16.3%). Most patients presented in SCAI Stage E (50%), followed by C (30%), D (17.5%), and B (2.1%). Vasopressors were used in 97.5%, and 36.5% were transferred from outside facilities. Temporary MCS was utilized in 50%, with Impella CP (34.6%) most common, followed by Impella 5.5 (30.8%), IABP (26.9%), Impella RP (3.8%), and VA-ECMO (3.8%). The mean lactate level across the cohort was 4.2 mmol/L, and the mean ALT was 285.57 U/L, suggesting evidence of systemic hypoperfusion and hepatic congestion. The average left ventricular ejection fraction (EF) was 28.7%, consistent with moderate systolic dysfunction. Notably, 50% of patients underwent pulmonary artery (PA) catheter placement during their evaluation. Despite high transfer rates, in-hospital mortality was 35.7%, below national averages for non-LVAD centers.
Conclusion: Implementation of a structured, interdisciplinary shock team protocol at a resource-limited center led to favorable outcomes in cardiogenic shock. Timely escalation, protocol-driven MCS use, and coordinated care can enable non-LVAD centers to deliver high-quality shock management.
Methods: We performed a retrospective review of adult patients with cardiogenic shock admitted between 2024–2025. Inclusion required ≥2 of the following: MAP <60 mmHg or a ≥30 mmHg drop from baseline, SBP <90 mmHg or ≥30 mmHg drop from baseline, HR >100 bpm, cardiac index less than 2.2 L per min per m2, PAPI <1.0, cardiac power output <0.6 W, or vasopressor/MCS requirement. Clinical, hemodynamic, and echocardiographic data were extracted from electronic records. The primary outcome was in-hospital mortality; secondary outcomes included MCS use, escalation timing, and transfer rate.
Results: A total of 40 patients were included (mean age 59.3 ± 13.6 years). The leading etiology was acute decompensated heart failure (51.2%), followed by NSTEMI (20.9%) and STEMI (16.3%). Most patients presented in SCAI Stage E (50%), followed by C (30%), D (17.5%), and B (2.1%). Vasopressors were used in 97.5%, and 36.5% were transferred from outside facilities. Temporary MCS was utilized in 50%, with Impella CP (34.6%) most common, followed by Impella 5.5 (30.8%), IABP (26.9%), Impella RP (3.8%), and VA-ECMO (3.8%). The mean lactate level across the cohort was 4.2 mmol/L, and the mean ALT was 285.57 U/L, suggesting evidence of systemic hypoperfusion and hepatic congestion. The average left ventricular ejection fraction (EF) was 28.7%, consistent with moderate systolic dysfunction. Notably, 50% of patients underwent pulmonary artery (PA) catheter placement during their evaluation. Despite high transfer rates, in-hospital mortality was 35.7%, below national averages for non-LVAD centers.
Conclusion: Implementation of a structured, interdisciplinary shock team protocol at a resource-limited center led to favorable outcomes in cardiogenic shock. Timely escalation, protocol-driven MCS use, and coordinated care can enable non-LVAD centers to deliver high-quality shock management.
More abstracts on this topic:
AI-Assisted Transseptal Puncture: Visual-Prompt Fine-Tuning of Foundation Models on Low-Dose X-RAY Images
Qi Xiuyu, Wang Xingyao, Cui Chang, Ju Weizhu, Chen Minglong
Artificial Intelligence ECG Model To Reduce False-Positive STEMI Alerts in the Emergency DepartmentDavis Adam, Mesbah Heba, Boone Stephen