Final ID: MP489
Impact of the COVID-19 Pandemic on Cardiovascular Mortality Trends and Place of Death in Patients with Diabetes Mellitus (2018-2023): A Nationwide Analysis
Abstract Body (Do not enter title and authors here):
Background: The COVID-19 pandemic disrupted healthcare systems and significantly impacted individuals with chronic conditions.
Research Question: What was the impact of the pandemic on diabetes mellitus (DM) as a contributing condition on cardiovascular disease (CVD) mortality trends and place of death?
Methods: Using the CDC WONDER database (2018–2023), we identified deaths due to CVD (ICD-10 codes: I00–I99) in individuals with DM (ICD-10 codes: E10-E14) in the United States. The study was divided into pre-COVID (2018-2019), during COVID (2020-2021), and post-COVID (2022-2023) periods. Age-adjusted mortality rates (AAMRs) per 100,000 population were stratified by age, sex, race/ethnicity, and regions. Places of death were classified as inpatient, outpatient/ER, home, hospice, or nursing home/long-term care.
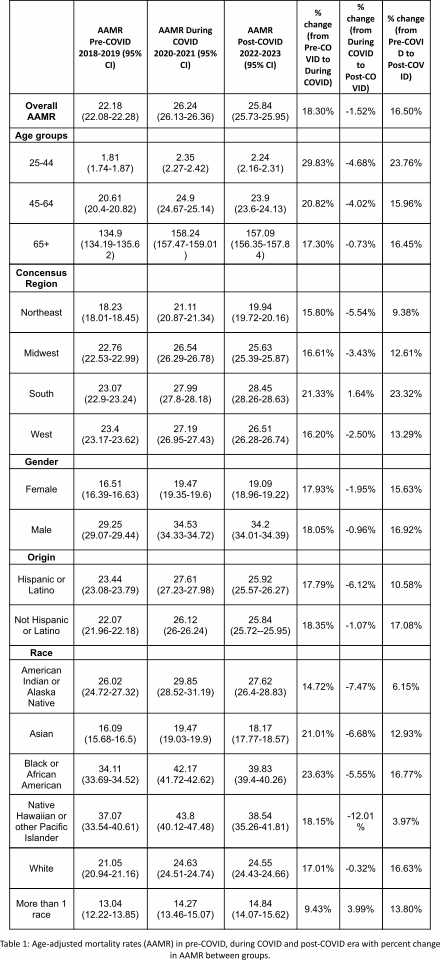
Results: There were a total of 617,414 deaths due to CVD in patients with DM and the AAMR increased from 22.18 per 100,000 pre-COVID to 26.24 during COVID and remained high at 25.84 post-COVID. AAMR increased across all age groups during the pandemic, with the most increase among adults aged 25-44 (+29.8%), followed by 45-64 (+20.8%) and ≥65 (+17.3%) which decreased by 4.68%, 4.02% and 0.73% post-COVID respectively (Table 1).
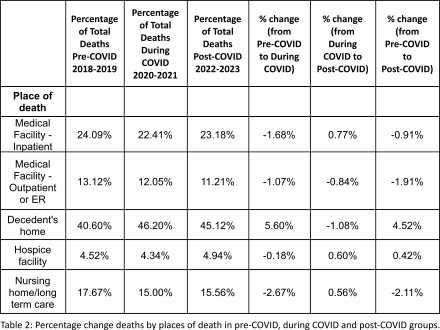
Home deaths increased considerably from 40.6% (69,344 of 170,777) pre-COVID to 46.2% (94,512 of 204,566) during COVID-19, with a slight decline to 45.1% (94,020 of 208,388) post-COVID. In contrast, deaths in nursing homes (−2.67%), outpatient/ER settings (−1.07%), and inpatient (−1.68%) declined during COVID.
Regionally, the South had greatest increase in AAMR (+21.3%) which increased to (+23.2%) post-COVID, followed by the West (+16.2% to +13.3%), Midwest (+16.6% to 12.6%), and Northeast (+15.8% to +9.4). Males and females had a comparable mortality increase during the pandemic (+18% and 17.9%) while non-Hispanic individuals had a higher increase in AAMR (+17.1%) as compared to Hispanics (+10.6%). Among races, Black individuals had the highest AAMR increase (+23.6%), followed by Asian (+21%), White (+17%), and American Indian or Alaska Native (+6.2%).
Conclusion: The COVID-19 pandemic was associated with considerable rise in CVD mortality in patients with DM, especially younger adults. This trend continued post-COVID and a considerable and lasting shift in place of death toward home settings was observed. These disparities underscore systemic gaps in prevention and chronic disease management that were magnified during the pandemic.
Background: The COVID-19 pandemic disrupted healthcare systems and significantly impacted individuals with chronic conditions.
Research Question: What was the impact of the pandemic on diabetes mellitus (DM) as a contributing condition on cardiovascular disease (CVD) mortality trends and place of death?
Methods: Using the CDC WONDER database (2018–2023), we identified deaths due to CVD (ICD-10 codes: I00–I99) in individuals with DM (ICD-10 codes: E10-E14) in the United States. The study was divided into pre-COVID (2018-2019), during COVID (2020-2021), and post-COVID (2022-2023) periods. Age-adjusted mortality rates (AAMRs) per 100,000 population were stratified by age, sex, race/ethnicity, and regions. Places of death were classified as inpatient, outpatient/ER, home, hospice, or nursing home/long-term care.
Results: There were a total of 617,414 deaths due to CVD in patients with DM and the AAMR increased from 22.18 per 100,000 pre-COVID to 26.24 during COVID and remained high at 25.84 post-COVID. AAMR increased across all age groups during the pandemic, with the most increase among adults aged 25-44 (+29.8%), followed by 45-64 (+20.8%) and ≥65 (+17.3%) which decreased by 4.68%, 4.02% and 0.73% post-COVID respectively (Table 1).
Home deaths increased considerably from 40.6% (69,344 of 170,777) pre-COVID to 46.2% (94,512 of 204,566) during COVID-19, with a slight decline to 45.1% (94,020 of 208,388) post-COVID. In contrast, deaths in nursing homes (−2.67%), outpatient/ER settings (−1.07%), and inpatient (−1.68%) declined during COVID.
Regionally, the South had greatest increase in AAMR (+21.3%) which increased to (+23.2%) post-COVID, followed by the West (+16.2% to +13.3%), Midwest (+16.6% to 12.6%), and Northeast (+15.8% to +9.4). Males and females had a comparable mortality increase during the pandemic (+18% and 17.9%) while non-Hispanic individuals had a higher increase in AAMR (+17.1%) as compared to Hispanics (+10.6%). Among races, Black individuals had the highest AAMR increase (+23.6%), followed by Asian (+21%), White (+17%), and American Indian or Alaska Native (+6.2%).
Conclusion: The COVID-19 pandemic was associated with considerable rise in CVD mortality in patients with DM, especially younger adults. This trend continued post-COVID and a considerable and lasting shift in place of death toward home settings was observed. These disparities underscore systemic gaps in prevention and chronic disease management that were magnified during the pandemic.
More abstracts on this topic:
Adiponectin and Adiponectin/Leptin Ratio Associate with Cardiometabolic Risk in South Asian Americans: Updates from the MASALA Study
Uttarwar Salil, Shah Nilay, Kanaya Alka, Gadgil Meghana
A Novel Approach to Manage Hypercholesterolemia: The Veterans Affairs Lipid Optimization Reimagined Quality Improvement (VALOR-QI) ProgramDjousse Luc, Leesch Tharen, Pena David, Gaziano Michael, Ward Rachel, Wellman Helen, Yel Nedim, Santos Abigail, Delgrande Jen, Fink Abigail, Colson Kristin, Pan Eddie