Final ID: MP487
The Impact of COVID-19 pandemic on Mortality and Place of Death among Patients with Ischemic Heart Disease in the United States (2018–2023): A nationwide analysis
Abstract Body (Do not enter title and authors here): Background: The COVID-19 pandemic disrupted health care systems and emergency care access across the United States.
Research Question: What was the impact of COVID-19 on mortality of patients with IHD and their places of death?
Methods: We used the CDC WONDER database to identify deaths due to IHD (ICD-10 codes I20-I25) from 2018-2023. The study was divided into pre-COVID (2018–2019), during COVID (2020–2021), and post-COVID (2022–2023) periods. Deaths were categorized by place of death: inpatient, outpatient or ER, decedent’s home, hospice facility, and nursing home/long term care. Adjusted mortality rates (AAMRs) per 100,000 population were stratified by age, sex, race, ethnicity and region.
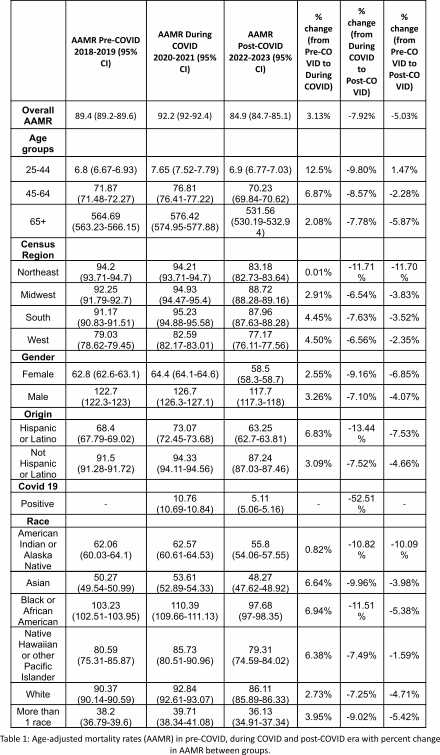
Results: Overall, 2,205,804 individuals died due to IHD and the AAMR increased from 89.4 per 100,000 pre-COVID to 92.2 during COVID, before declining to 84.9 in the post-COVID era. AAMR for individuals having concomitant IHD and Covid-19 decreased by 52.5% from 10.76 during the pandemic to 5.11 after the pandemic. (Table 1)
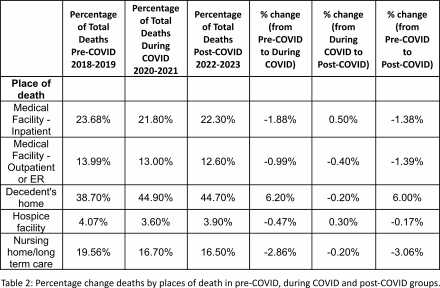
Place of death analysis revealed substantial shift toward home deaths during the pandemic which increased from 38.7% (264,005 of 682,196) to 44.9% (318,249 of 708,342) during COVID, remaining elevated post-COVID (44.7%). Inpatient deaths fell from 23.6% to 21.8% during COVID and Deaths in outpatient/ER (14.0% to 13%), nursing homes (19.5% to 16.7%), and hospice (4.0% to 3.6%) also declined. (Table 2)
Young adults aged 25-44 had the largest AAMR rise during COVID (+12.5%), with smaller increases in those aged 45-64 (+6.9%) and ≥65 (+2.1%). Geographically, AAMR increased the highest in the South and West (+4.5%) with greatest post-COVID declines in the Northeast (-11.7%).
Hispanic individuals saw a 6.8% increase in AAMR during COVID and a 13.4% decline after. Increases in AAMR during COVID were highest among Black (+6.9%), Asian (+6.6%), and Pacific Islander (+6.4%) individuals, while White individuals had a smaller rise (+2.7%).
Conclusion: COVID-19 pandemic was associated with a temporary rise in IHD mortality and a substantial shift in place of death toward home, which continued post-COVID. Although overall IHD mortality declined post-pandemic, this recovery was uneven across age, race, and region. This highlights persistent disparities and long-term changes in healthcare utilization and end-of-life care patterns following the pandemic and underscore the urgent need for targeted interventions to improve healthcare access.
Research Question: What was the impact of COVID-19 on mortality of patients with IHD and their places of death?
Methods: We used the CDC WONDER database to identify deaths due to IHD (ICD-10 codes I20-I25) from 2018-2023. The study was divided into pre-COVID (2018–2019), during COVID (2020–2021), and post-COVID (2022–2023) periods. Deaths were categorized by place of death: inpatient, outpatient or ER, decedent’s home, hospice facility, and nursing home/long term care. Adjusted mortality rates (AAMRs) per 100,000 population were stratified by age, sex, race, ethnicity and region.
Results: Overall, 2,205,804 individuals died due to IHD and the AAMR increased from 89.4 per 100,000 pre-COVID to 92.2 during COVID, before declining to 84.9 in the post-COVID era. AAMR for individuals having concomitant IHD and Covid-19 decreased by 52.5% from 10.76 during the pandemic to 5.11 after the pandemic. (Table 1)
Place of death analysis revealed substantial shift toward home deaths during the pandemic which increased from 38.7% (264,005 of 682,196) to 44.9% (318,249 of 708,342) during COVID, remaining elevated post-COVID (44.7%). Inpatient deaths fell from 23.6% to 21.8% during COVID and Deaths in outpatient/ER (14.0% to 13%), nursing homes (19.5% to 16.7%), and hospice (4.0% to 3.6%) also declined. (Table 2)
Young adults aged 25-44 had the largest AAMR rise during COVID (+12.5%), with smaller increases in those aged 45-64 (+6.9%) and ≥65 (+2.1%). Geographically, AAMR increased the highest in the South and West (+4.5%) with greatest post-COVID declines in the Northeast (-11.7%).
Hispanic individuals saw a 6.8% increase in AAMR during COVID and a 13.4% decline after. Increases in AAMR during COVID were highest among Black (+6.9%), Asian (+6.6%), and Pacific Islander (+6.4%) individuals, while White individuals had a smaller rise (+2.7%).
Conclusion: COVID-19 pandemic was associated with a temporary rise in IHD mortality and a substantial shift in place of death toward home, which continued post-COVID. Although overall IHD mortality declined post-pandemic, this recovery was uneven across age, race, and region. This highlights persistent disparities and long-term changes in healthcare utilization and end-of-life care patterns following the pandemic and underscore the urgent need for targeted interventions to improve healthcare access.
More abstracts on this topic:
A Contemporary Machine Learning-Based Risk Stratification for Mortality and Hospitalization in Heart Failure with Preserved Ejection Fraction Using Multimodal Real-World Data
Fudim Marat, Weerts Jerremy, Patel Manesh, Balu Suresh, Hintze Bradley, Torres Francisco, Micsinai Balan Mariann, Rigolli Marzia, Kessler Paul, Touzot Maxime, Lund Lars, Van Empel Vanessa, Pradhan Aruna, Butler Javed, Zehnder Tobias, Sauty Benoit, Esposito Christian, Balazard Félix, Mayer Imke, Hallal Mohammad, Loiseau Nicolas
A 60-fold increase in SCA risk in the last kilometer of endurance races : Final sprint, fatal outcome.Chocron Richard, Levy Bernard, Beganton Franckie, Bougouin Wulfran, Empana Jean-philippe, Jouven Xavier, Laurenceau Thomas, Chabrol Marion, Mignot Soline, Meli Ugo, Langlois Camille, Cezard Pierre, Schwartz Peter, Kaab Stefan