Final ID: MP163
Multi-Modality Imaging in Giant Cell Myocarditis
Abstract Body (Do not enter title and authors here): Background:
Giant cell myocarditis (GCM) is a rare autoimmune cardiomyopathy that leads to fulminant heart failure. Diagnosis remains challenging, with many patients presenting late in their disease course.
Case:
A previously healthy 48-year-old man presented to his clinic with a two-week history of palpitations after a camping trip without insect bites or illnesses. He denied significant medical conditions, or a personal or family history of syncope, heart disease, or sudden death.
Outpatient cardiac rhythm monitoring demonstrated multi-focal premature ventricular contraction (PVC) burden of 30% and a 1-minute episode of sustained monomorphic ventricular tachycardia (VT) at 200 bpm, prompting hospitalization.
Admission vitals were stable, and physical exam was negative for signs of heart failure. An initial ECG showed accelerated idioventricular rhythm with multiple QRS morphologies. Troponin, inflammatory markers, and chemistry panel were normal. Transthoracic echocardiogram showed ventricular ectopy with a left ventricular ejection fraction of 50%, without any other pathology.
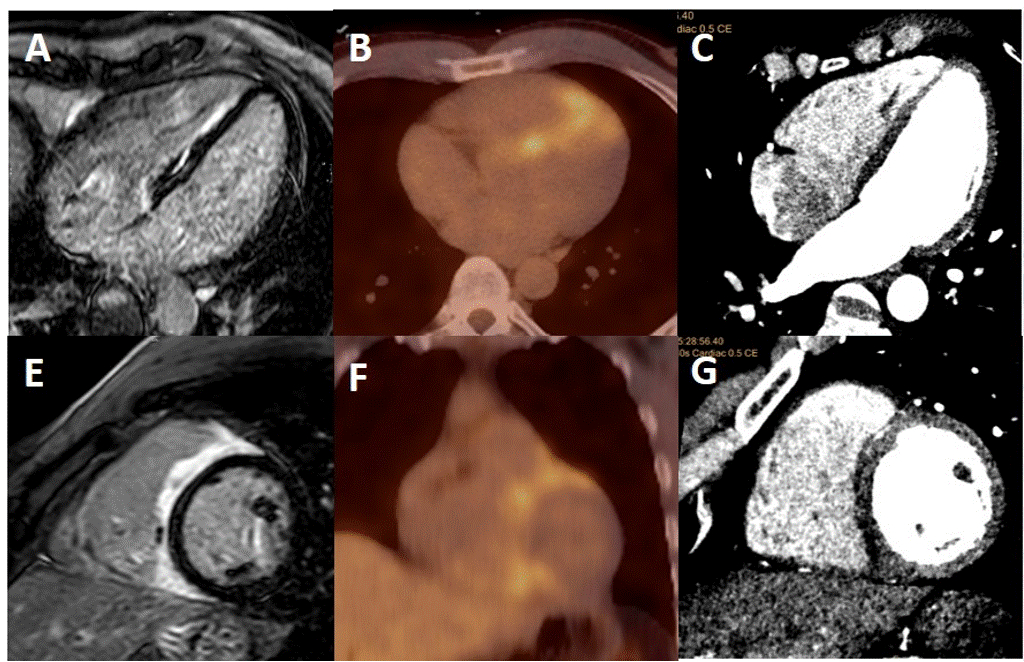
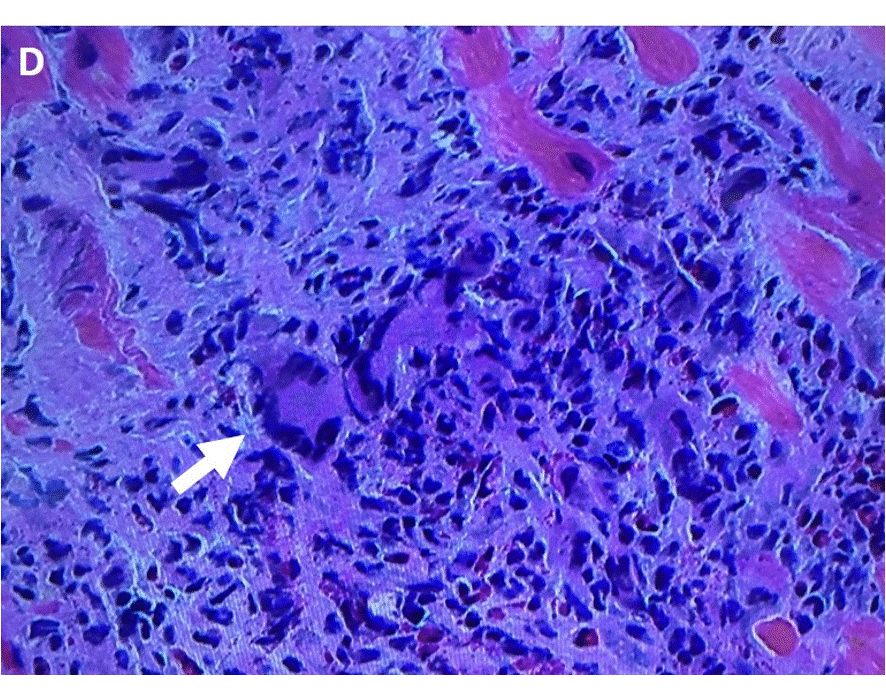
Cardiac MRI (cMRI) demonstrated late gadolinium enhancement (LGE) in the right ventricular aspect of the interventricular septum on T1 sequences not confined to a typical coronary territory. Positron emission tomography (PET) with fludeoxyglucose (18F-FDG) showed increased avidity in the same region without extracardiac uptake. A coronary computed tomography (CT) angiogram also showed decreased attenuation of the same region without CAD or coronary anomalies. Pathology from an endomyocardial biopsy showed dense lymphocytic and eosinophilic infiltrate with multinucleated giant cells without granulomas, consistent with GCM.
Sotalol was initiated to suppress ventricular ectopy while pathology was pending but was ineffective. The patient was switched to amiodarone. After diagnosis of GCM, the patient received prednisone and cyclosporine. A subcutaneous ICD was implanted prior to discharge.
Three months later, the patient was appropriately shocked for sustained VT. Repeat PET had unchanged FDG-avidity, for which mycophenolate was added. Six-month follow-up was negative for ventricular arrhythmias. Repeat PET demonstrated complete resolution of FDG-avidity.
Discussion:
GCM requires prompt diagnosis and treatment to prevent mortality and morbidity. While endomyocardial biopsy remains the gold standard for diagnosis, non-invasive imaging allows for earlier diagnosis and assessment of response.
Giant cell myocarditis (GCM) is a rare autoimmune cardiomyopathy that leads to fulminant heart failure. Diagnosis remains challenging, with many patients presenting late in their disease course.
Case:
A previously healthy 48-year-old man presented to his clinic with a two-week history of palpitations after a camping trip without insect bites or illnesses. He denied significant medical conditions, or a personal or family history of syncope, heart disease, or sudden death.
Outpatient cardiac rhythm monitoring demonstrated multi-focal premature ventricular contraction (PVC) burden of 30% and a 1-minute episode of sustained monomorphic ventricular tachycardia (VT) at 200 bpm, prompting hospitalization.
Admission vitals were stable, and physical exam was negative for signs of heart failure. An initial ECG showed accelerated idioventricular rhythm with multiple QRS morphologies. Troponin, inflammatory markers, and chemistry panel were normal. Transthoracic echocardiogram showed ventricular ectopy with a left ventricular ejection fraction of 50%, without any other pathology.
Cardiac MRI (cMRI) demonstrated late gadolinium enhancement (LGE) in the right ventricular aspect of the interventricular septum on T1 sequences not confined to a typical coronary territory. Positron emission tomography (PET) with fludeoxyglucose (18F-FDG) showed increased avidity in the same region without extracardiac uptake. A coronary computed tomography (CT) angiogram also showed decreased attenuation of the same region without CAD or coronary anomalies. Pathology from an endomyocardial biopsy showed dense lymphocytic and eosinophilic infiltrate with multinucleated giant cells without granulomas, consistent with GCM.
Sotalol was initiated to suppress ventricular ectopy while pathology was pending but was ineffective. The patient was switched to amiodarone. After diagnosis of GCM, the patient received prednisone and cyclosporine. A subcutaneous ICD was implanted prior to discharge.
Three months later, the patient was appropriately shocked for sustained VT. Repeat PET had unchanged FDG-avidity, for which mycophenolate was added. Six-month follow-up was negative for ventricular arrhythmias. Repeat PET demonstrated complete resolution of FDG-avidity.
Discussion:
GCM requires prompt diagnosis and treatment to prevent mortality and morbidity. While endomyocardial biopsy remains the gold standard for diagnosis, non-invasive imaging allows for earlier diagnosis and assessment of response.
More abstracts on this topic:
A Comparison of Characteristics and Outcomes in Patients with and without Adult Congenital Heart Disease Undergoing Catheter Ablation for Ventricular Tachycardia
Futela Pragyat, Poddar Aastha, Kowlgi Gurukripa
A Case of Caseous Mitral Annular Calcification and the Utility of Multimodality Cardiac ImagingNguyen Amanda, English Carter, Ghasemiesfe Ahmadreza, Venugopal Sandhya