Final ID: MP428
Nocturnal Very Low Frequency of Heart Rate Variability Predicts Adverse Cardiovascular Events in Obese Individuals
Abstract Body (Do not enter title and authors here): Background: The risk of major adverse cardiovascular and cerebrovascular events (MACCEs) in obese individuals is often assessed by hypoxia and hypopnea levels, while heart rate variability (HRV) has not been widely studied in this population.
Aims: To study the association between HRV and MACCEs in patients with obesity.
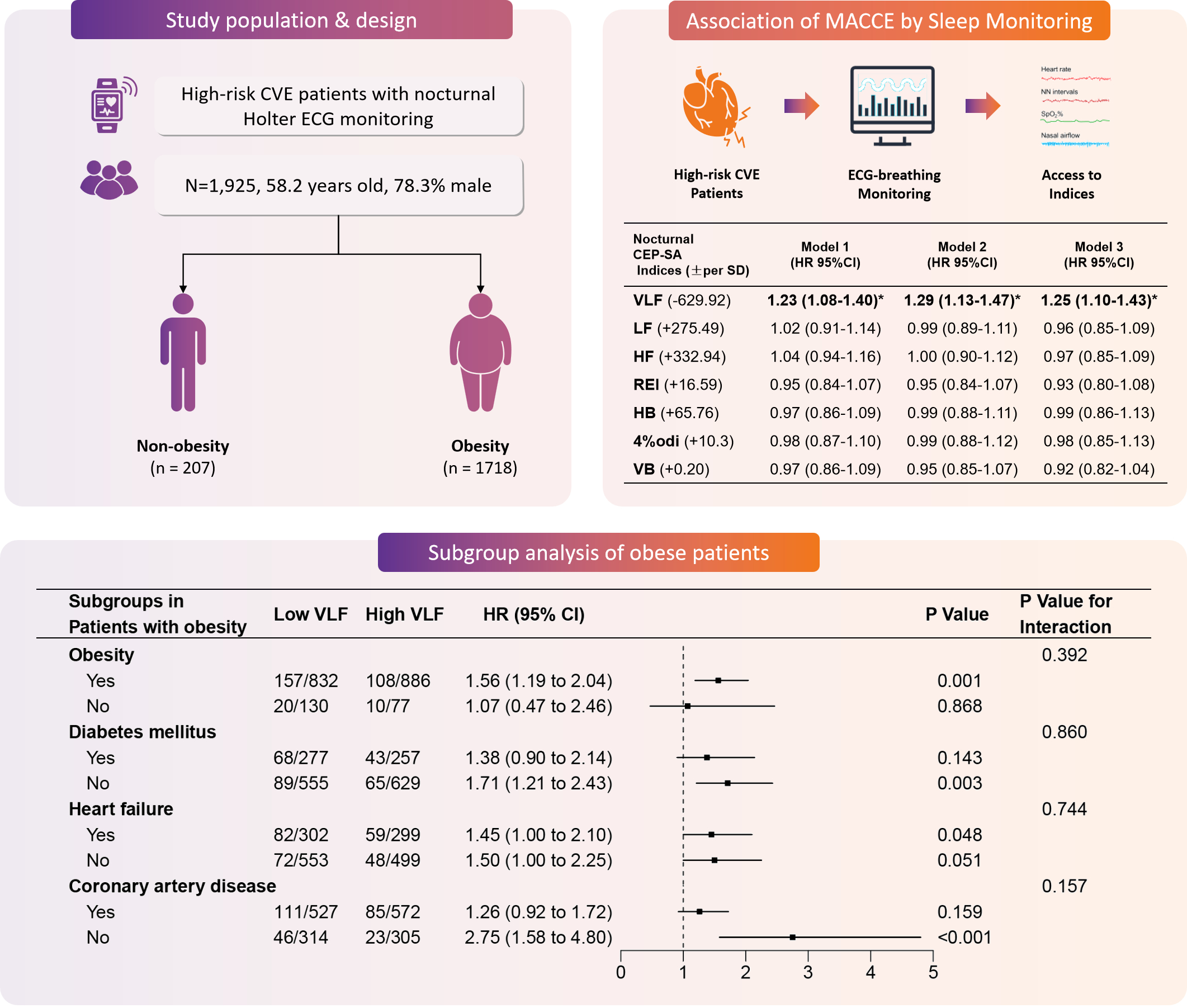
Methods: This prospective cohort included 1925 patients undergoing nocturnal Holter electrocardiographic monitoring and home sleep apnea test (HSAT) from 2017–2021. Obesity was defined as excess for body mass index (BMI) and one measurement of body size (waist circumference, waist-to-hip ratio and waist-to-height ratio), or excess for two measurements of body size regardless of BMl. Nocturnal HRV indices were obtained from variation in the normal-to-normal intervals and divided into 3 subtypes based on frequency-domain spectrum, i.e., high frequency (HF, 0.15–0.5 Hz), low frequency (LF, 0.04–0.15 Hz), and very low frequency (VLF, 0.0033–0.04 Hz). Hypoxic burden and ventilation burden indices were recorded by HSAT monitors. Low VLF level was defined as a VLF of < the median value. Predictive values of HRV, hypoxia burden and ventilation burden indices were assessed with Cox regression. Sensitivity analysis was performed in obese patients (n=1718, 89.2%) to assess if the association between VLF and MACCEs was modified by diabetes mellitus (DM) (n=534), heart failure (n=601), and coronary artery disease (CAD) (n=1099).
Results: Mean age was 58.2±11.5 years (78.3% men). Median follow-up was 3.1 years. MACCEs occurred in 15.3% (295/1925). Patients with decreased per VLF standard deviation (629.92 ms2) had a higher cumulative risk of MACCEs (adjusted hazard ratio [aHR] 1.25, 95% confidence interval [CI], 1.10–1.43, P=0.001). Neither other HRV indices nor indices of hypoxia and ventilation burdens were correlated with MACCEs (P>0.05). In obese patients, the association of low VLF level with MACCEs was observed in those without DM (aHR 1.71, 95% CI 1.21–2.43, P=0.003), with heart failure (aHR 1.45, 95% CI 1.00–2.10, P<0.048), and without CAD (aHR 2.75, 95% CI 1.58–4.80, P<0.001). No significant interaction was found among subgroups of DM, CAD and heart failure (P for interaction > 0.05).
Conclusion: Reduced nocturnal VLF was linked to increased risk of MACCE in obese patients. The results of this study highlight the importance and argue for the necessity of monitoring nocturnal VLF in cardiovascular risk assessment for obese individuals.
Aims: To study the association between HRV and MACCEs in patients with obesity.
Methods: This prospective cohort included 1925 patients undergoing nocturnal Holter electrocardiographic monitoring and home sleep apnea test (HSAT) from 2017–2021. Obesity was defined as excess for body mass index (BMI) and one measurement of body size (waist circumference, waist-to-hip ratio and waist-to-height ratio), or excess for two measurements of body size regardless of BMl. Nocturnal HRV indices were obtained from variation in the normal-to-normal intervals and divided into 3 subtypes based on frequency-domain spectrum, i.e., high frequency (HF, 0.15–0.5 Hz), low frequency (LF, 0.04–0.15 Hz), and very low frequency (VLF, 0.0033–0.04 Hz). Hypoxic burden and ventilation burden indices were recorded by HSAT monitors. Low VLF level was defined as a VLF of < the median value. Predictive values of HRV, hypoxia burden and ventilation burden indices were assessed with Cox regression. Sensitivity analysis was performed in obese patients (n=1718, 89.2%) to assess if the association between VLF and MACCEs was modified by diabetes mellitus (DM) (n=534), heart failure (n=601), and coronary artery disease (CAD) (n=1099).
Results: Mean age was 58.2±11.5 years (78.3% men). Median follow-up was 3.1 years. MACCEs occurred in 15.3% (295/1925). Patients with decreased per VLF standard deviation (629.92 ms2) had a higher cumulative risk of MACCEs (adjusted hazard ratio [aHR] 1.25, 95% confidence interval [CI], 1.10–1.43, P=0.001). Neither other HRV indices nor indices of hypoxia and ventilation burdens were correlated with MACCEs (P>0.05). In obese patients, the association of low VLF level with MACCEs was observed in those without DM (aHR 1.71, 95% CI 1.21–2.43, P=0.003), with heart failure (aHR 1.45, 95% CI 1.00–2.10, P<0.048), and without CAD (aHR 2.75, 95% CI 1.58–4.80, P<0.001). No significant interaction was found among subgroups of DM, CAD and heart failure (P for interaction > 0.05).
Conclusion: Reduced nocturnal VLF was linked to increased risk of MACCE in obese patients. The results of this study highlight the importance and argue for the necessity of monitoring nocturnal VLF in cardiovascular risk assessment for obese individuals.
More abstracts on this topic:
Forecasting Mortality Associated with Obstructive Sleep Apnea and Sudden Cardiac Death Among Older Adults in the U.S. (1999–2035) Using Machine Learning Models.
Zafar Amna, Umar Muhammad, Ali Syed Awab, Habib Huzefa, Shamim Laiba, Hidayat Ayesha, Bareeqa Syeda Beenish, Noori Muhammad Atif Masood, Vasudev Rahul
Comparative Analysis of ECG Processing Software Performance on Traditional vs Patch-Based Lead II ConfigurationsDeery Adrian, Dowie Danielle, Diven Jordan, Easlea Holly