Final ID: MP93
Decreased Nocturnal Very Low Frequency of Heart Rate Variability Linked to Adverse Cardiovascular Events in Patients with Hypertension
Abstract Body (Do not enter title and authors here): Background: Evaluating nocturnal regulation of cardiac autonomic nervous system (CANS) with frequency-domain heart rate variability (HRV) is relevant, especially in patients with sleep apnea. So far, the association between very low frequency (VLF) of HRV and major adverse cardiovascular and cerebrovascular events (MACCEs) has not been sufficiently elucidated.
Aims: We seek to evaluate the impact of VLF of HRV on MACCEs in patients with hypertension.
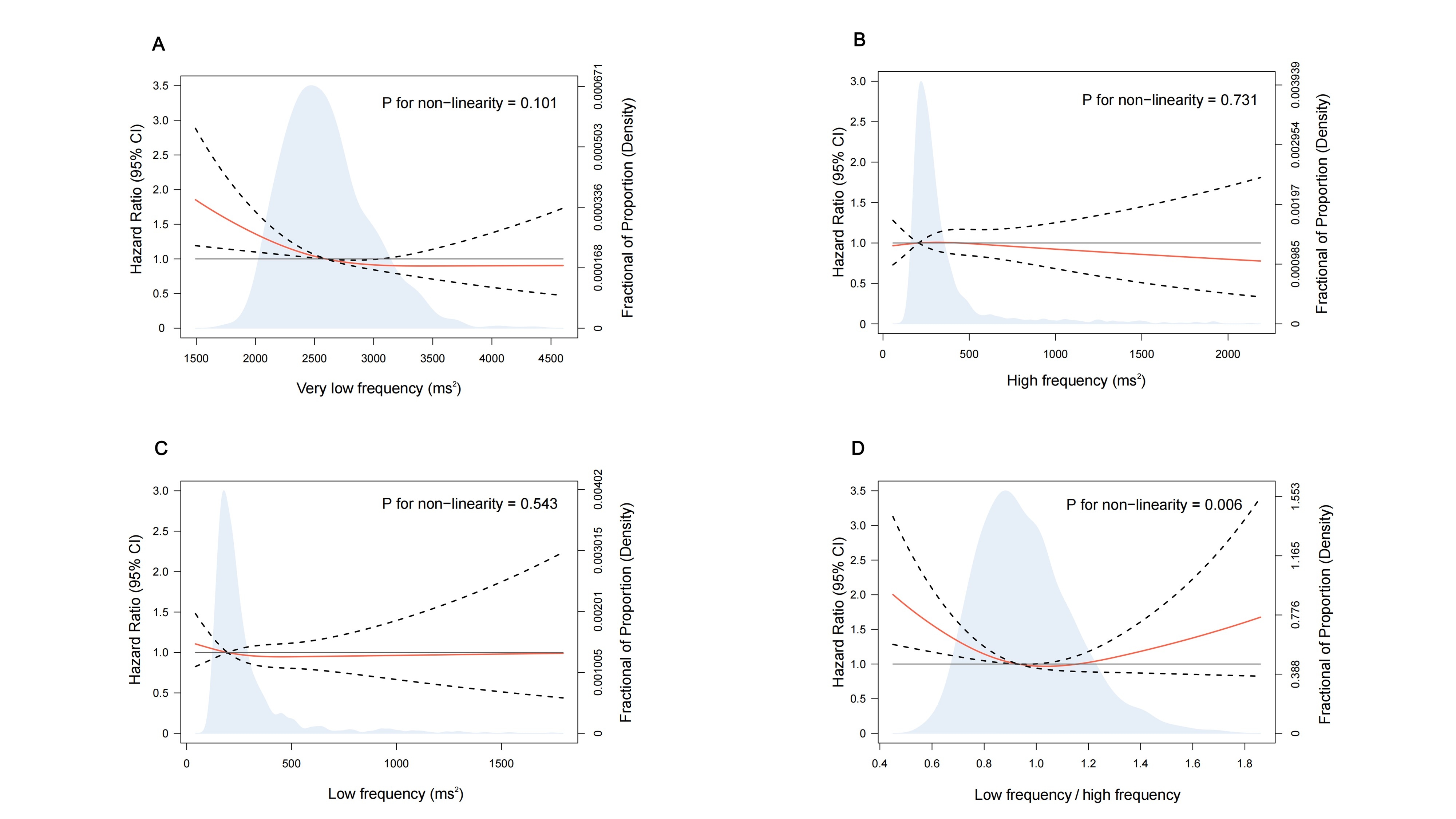
Methods: This prospective study enrolled 2,061 hypertensive patients from 2017–2021 monitored with nocturnal Holter electrocardiography and type III home sleep apnea testing. Nocturnal HRV was defined by the variation in normal-to-normal intervals at night, and evaluated based on frequency-domain spectra, including high frequency (HF) (0.15–0.5 Hz), low frequency (LF) (0.04–0.15 Hz), VLF (0.0033–0.04 Hz), and the LF/HF ratio. Restricted cubic spline analysis via Cox regression was used to explore the prognostic effects of different HRV indices. The cut-off point for VLF was set at 2,566 ms2. Stabilized inverse probability weighting (IPW) based on propensity scores was used to balance baseline characteristics between low-VLF (<2566 ms2) and high-VLF groups (≥2566 ms2).
Results: Over a median follow-up of 39 months, 1,867 patients aged 58.4±11.2 years (77.4% men) were included in final analysis. MACCEs occurred in 15.3%. Among 4 HRV indices, only VLF showed a stable nonlinear prognostic association. Compared with patients with high-VLF group, the low-VLF group had a 42–47% higher risk of MACCEs compared to the high-VLF group, depending on the cohort (unadjusted or IPW). In obese patients, those with low-VLF vs high-VLF showed an unadjusted HR of 1.55 for MACCEs (95% CI, 1.21–1.99; P=0.001), which persisted after IPW adjustment (HR 1.38 [95% CI, 1.06–1.81]; P=0.016). Similarly, patients with OSA in the low-VLF group (vs high-VLF group) had an increased risk of MACCEs (unadjusted HR 1.56, 95% CI 1.20–2.02, P=0.001; adjusted HR 1.38, 95% CI 1.07–1.77, P=0.013). The ratio of nocturnal-to-baseline VLF had an area under the curve (AUC) of 0.962 in predicting respiratory event-related cardiac cycle changes during short time intervals.
Conclusion: Lower nocturnal VLF of HRV may increase the risk of MACCEs in patients with hypertension, particularly those with obesity and sleep apnea. suggesting a pathophysiological mechanism that links cardiovascular events to impaired regulation of cardiopulmonary coupling by the CANS.
Aims: We seek to evaluate the impact of VLF of HRV on MACCEs in patients with hypertension.
Methods: This prospective study enrolled 2,061 hypertensive patients from 2017–2021 monitored with nocturnal Holter electrocardiography and type III home sleep apnea testing. Nocturnal HRV was defined by the variation in normal-to-normal intervals at night, and evaluated based on frequency-domain spectra, including high frequency (HF) (0.15–0.5 Hz), low frequency (LF) (0.04–0.15 Hz), VLF (0.0033–0.04 Hz), and the LF/HF ratio. Restricted cubic spline analysis via Cox regression was used to explore the prognostic effects of different HRV indices. The cut-off point for VLF was set at 2,566 ms2. Stabilized inverse probability weighting (IPW) based on propensity scores was used to balance baseline characteristics between low-VLF (<2566 ms2) and high-VLF groups (≥2566 ms2).
Results: Over a median follow-up of 39 months, 1,867 patients aged 58.4±11.2 years (77.4% men) were included in final analysis. MACCEs occurred in 15.3%. Among 4 HRV indices, only VLF showed a stable nonlinear prognostic association. Compared with patients with high-VLF group, the low-VLF group had a 42–47% higher risk of MACCEs compared to the high-VLF group, depending on the cohort (unadjusted or IPW). In obese patients, those with low-VLF vs high-VLF showed an unadjusted HR of 1.55 for MACCEs (95% CI, 1.21–1.99; P=0.001), which persisted after IPW adjustment (HR 1.38 [95% CI, 1.06–1.81]; P=0.016). Similarly, patients with OSA in the low-VLF group (vs high-VLF group) had an increased risk of MACCEs (unadjusted HR 1.56, 95% CI 1.20–2.02, P=0.001; adjusted HR 1.38, 95% CI 1.07–1.77, P=0.013). The ratio of nocturnal-to-baseline VLF had an area under the curve (AUC) of 0.962 in predicting respiratory event-related cardiac cycle changes during short time intervals.
Conclusion: Lower nocturnal VLF of HRV may increase the risk of MACCEs in patients with hypertension, particularly those with obesity and sleep apnea. suggesting a pathophysiological mechanism that links cardiovascular events to impaired regulation of cardiopulmonary coupling by the CANS.
More abstracts on this topic:
A Longitudinal 20-year Analysis Indicates Acceleration of Cardiometabolic Comorbidities on Dementia Risk
Lihua Huang, Danish Muhammad, Auyeung Tw, Jenny Lee, Kwok Timothy, Abrigo Jill, Wei Yingying, Lo Cecilia, Fung Erik
Acute Pressor, Chronotropic and Adrenergic Effects of Adderall - A Randomized Double-Blind Placebo Controlled Crossover StudySomers Kiran, Bock Joshua, Covassin Naima, Bukartyk Jan, Rajendran Aiswarya, Svatikova Anna