Final ID: MP84
Non-Bacterial Thrombotic Endocarditis and Intraventricular Small Vessel Thromboembolic Occlusion Mimicking ICI-Myocarditis in a Patient Treated with Pembrolizumab
Abstract Body (Do not enter title and authors here): Case Description:
Immune checkpoint inhibitors (ICIs) have transformed cancer therapy but are associated with immune-related adverse events, including cardiovascular toxicity. While ICI-myocarditis is rare but potentially fatal, thrombotic complications—such as venous thromboembolism, arterial occlusion, and non-bacterial thrombotic endocarditis (NBTE)—are underrecognized. These raise questions about the roles of malignancy-associated hypercoagulability versus ICI-induced effects. We present a case of NBTE and myocardial microthrombi mimicking ICI-myocarditis.
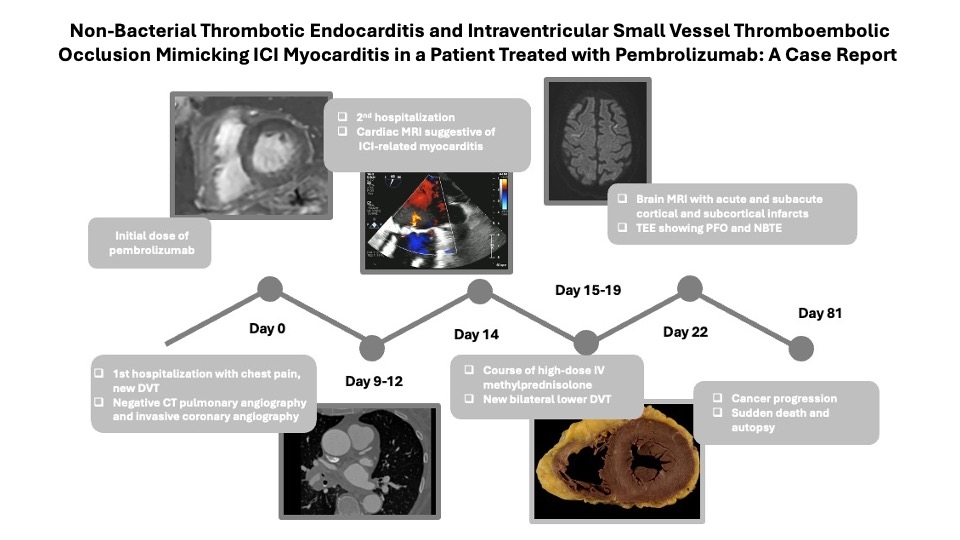
A 76-year-old woman with metastatic adenosquamous lung cancer and recent DVT (on apixaban and aspirin) presented with worsening dyspnea three weeks after starting pembrolizumab (Image 1). One week earlier, CT pulmonary angiography and coronary angiography were unrevealing. On presentation, she was stable but had peripheral edema, a late diastolic murmur, and elevated hs troponin (706→657→656 ng/L). NT-proBNP was 11,500 pg/mL. Cardiac MRI showed mid-wall late gadolinium enhancement (LGE), myocardial edema, and elevated T2 values—findings concerning for ICI-myocarditis. She initially improved on intravenous methylprednisolone.
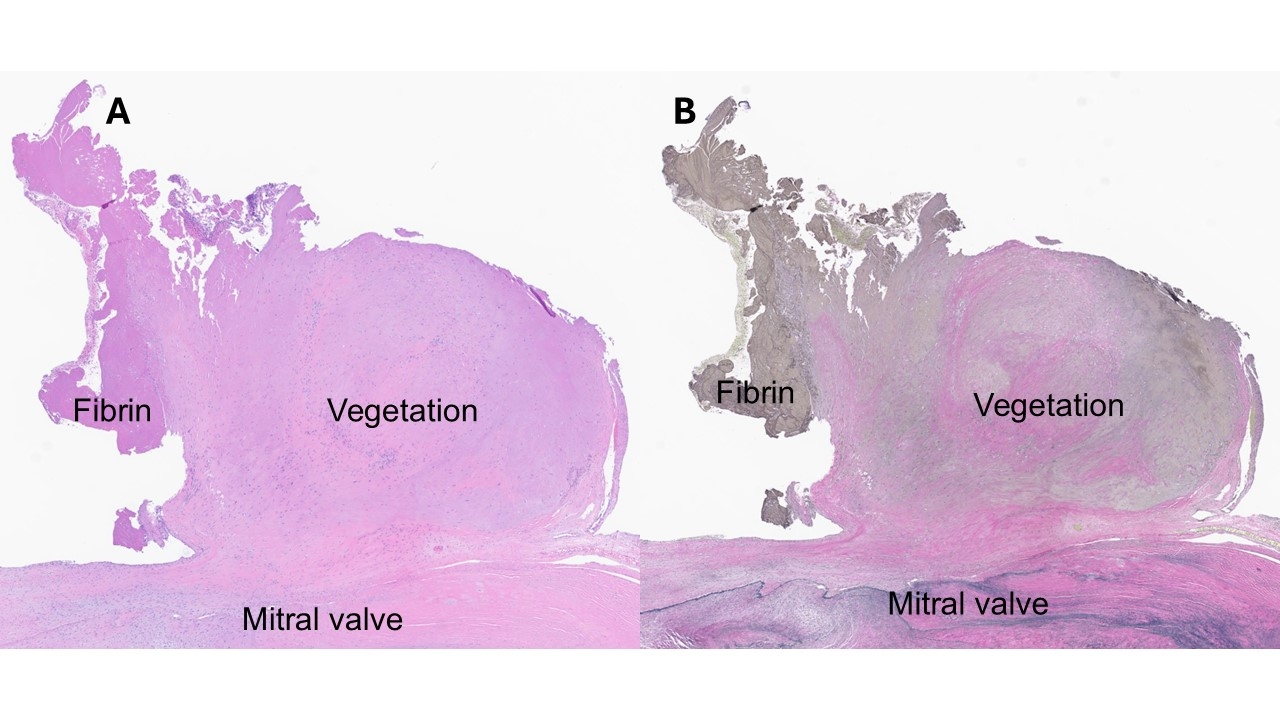
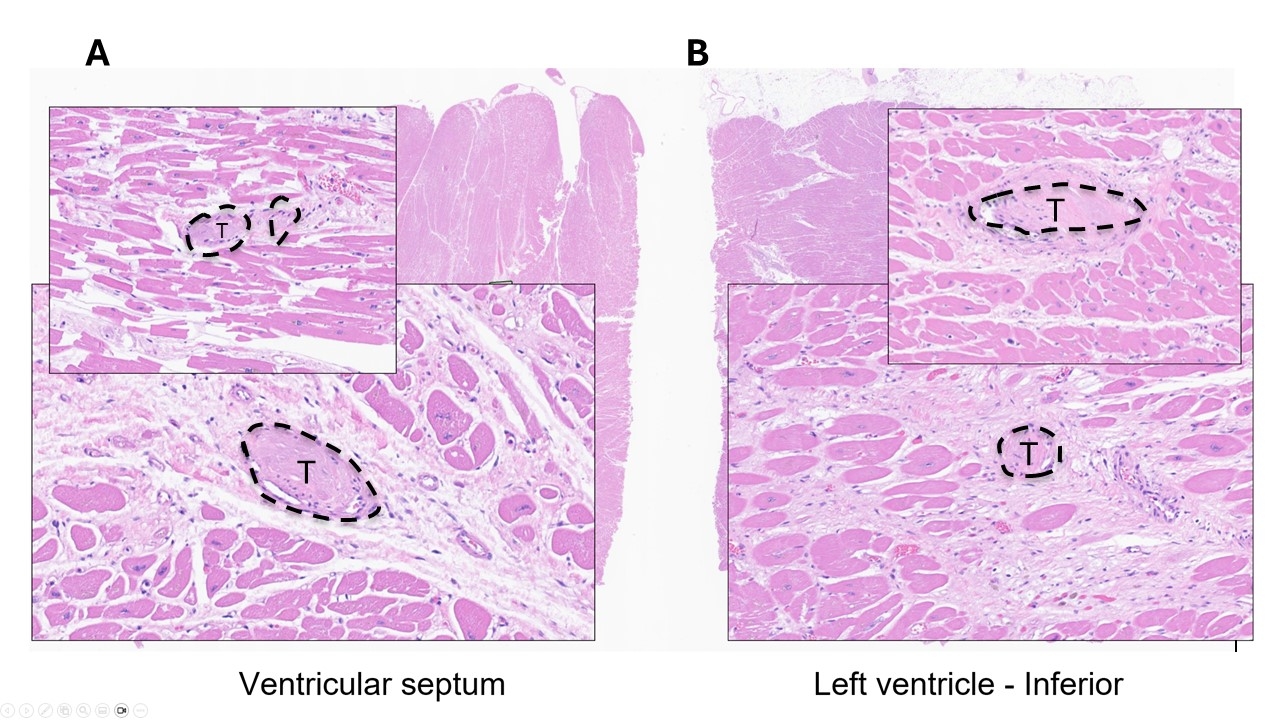
A week later, brain MRI showed multifocal embolic infarcts. Doppler ultrasound revealed a new left-sided DVT. TEE showed no intracardiac thrombus but identified a thickened aortic valve with moderate-to-severe regurgitation, a thickened mitral A2 segment with moderate regurgitation, and a patent foramen ovale (PFO) with left-to-right shunting. Findings raised concern for NBTE with systemic embolism or paradoxical embolism. Anticoagulation was transitioned to heparin, then warfarin. She was discharged on oral prednisone without further cancer therapy. Two months later, she died suddenly. Autopsy revealed fibrin-rich vegetations on the mitral valve consistent with NBTE and thromboembolic infarcts in small myocardial arteries, without inflammatory infiltrates or myocardial scarring (Image 2 and 3).
Conclusion:
This case highlights NBTE and microthrombi as important mimics of ICI-myocarditis. Despite MRI features suggestive of inflammation, pathology confirmed ischemic injury. ICIs have been suggested to promote thrombosis through elevated factor VIII, von Willebrand factor, reduced protein S, and systemic inflammation. Clinicians should consider thrombotic mimics in ICI-treated patients with cardiac symptoms and abnormal imaging. Tissue diagnosis may be necessary to guide management.
Immune checkpoint inhibitors (ICIs) have transformed cancer therapy but are associated with immune-related adverse events, including cardiovascular toxicity. While ICI-myocarditis is rare but potentially fatal, thrombotic complications—such as venous thromboembolism, arterial occlusion, and non-bacterial thrombotic endocarditis (NBTE)—are underrecognized. These raise questions about the roles of malignancy-associated hypercoagulability versus ICI-induced effects. We present a case of NBTE and myocardial microthrombi mimicking ICI-myocarditis.
A 76-year-old woman with metastatic adenosquamous lung cancer and recent DVT (on apixaban and aspirin) presented with worsening dyspnea three weeks after starting pembrolizumab (Image 1). One week earlier, CT pulmonary angiography and coronary angiography were unrevealing. On presentation, she was stable but had peripheral edema, a late diastolic murmur, and elevated hs troponin (706→657→656 ng/L). NT-proBNP was 11,500 pg/mL. Cardiac MRI showed mid-wall late gadolinium enhancement (LGE), myocardial edema, and elevated T2 values—findings concerning for ICI-myocarditis. She initially improved on intravenous methylprednisolone.
A week later, brain MRI showed multifocal embolic infarcts. Doppler ultrasound revealed a new left-sided DVT. TEE showed no intracardiac thrombus but identified a thickened aortic valve with moderate-to-severe regurgitation, a thickened mitral A2 segment with moderate regurgitation, and a patent foramen ovale (PFO) with left-to-right shunting. Findings raised concern for NBTE with systemic embolism or paradoxical embolism. Anticoagulation was transitioned to heparin, then warfarin. She was discharged on oral prednisone without further cancer therapy. Two months later, she died suddenly. Autopsy revealed fibrin-rich vegetations on the mitral valve consistent with NBTE and thromboembolic infarcts in small myocardial arteries, without inflammatory infiltrates or myocardial scarring (Image 2 and 3).
Conclusion:
This case highlights NBTE and microthrombi as important mimics of ICI-myocarditis. Despite MRI features suggestive of inflammation, pathology confirmed ischemic injury. ICIs have been suggested to promote thrombosis through elevated factor VIII, von Willebrand factor, reduced protein S, and systemic inflammation. Clinicians should consider thrombotic mimics in ICI-treated patients with cardiac symptoms and abnormal imaging. Tissue diagnosis may be necessary to guide management.
More abstracts on this topic:
Angiotensin II Infusion Promotes Splenic T Cell Response To Ex Vivo Polyclonal Activation In C57Bl/6J Mice
Dattmore Devon, Leipprandt Jeffrey R., Awali Saamera, Lauver Adam, Rockwell Cheryl
A Case of Steroid-Refractory Immune-checkpoint-inhibitor Induced Myocarditis Responsive to Mycophenolate and Anti-thymocyte globulinDabdoub Jorge, Wilson Michael, Gottbrecht Matthew, Salazar Ryan, Shih Jeffrey