Final ID: MP1706
Predictors of Mortality Among Elderly Patients Undergoing Redo Surgical Mitral Valve Replacement; a National Estimate in the United States
Abstract Body (Do not enter title and authors here): Introduction: Although redo surgical mitral valve replacement(redo-SMVR) is associated with a higher mortality risk compared to valve-in-valve transcatheter mitral valve replacement(ViV-TMVR), it is still frequently chosen due to various factors such as anatomical limitations and limited availability of ViV-TMVR expertise. We conducted this study to support the development of improved risk stratification protocols.
Methods: For this study, we considered patients aged 60 years or older who were hospitalized with a primary code for redo-SMVR through the National Inpatient Sample (NIS, 2016-2022). We adopted the methodologies set in prior studies and applied appropriate stratification and clustering of data. The all-cause mortality rates were estimated, and regression models were set up to estimate the adjusted odds ratio (aOR), 95% confidence intervals (95% CI), and p-values of clinically relevant variables.
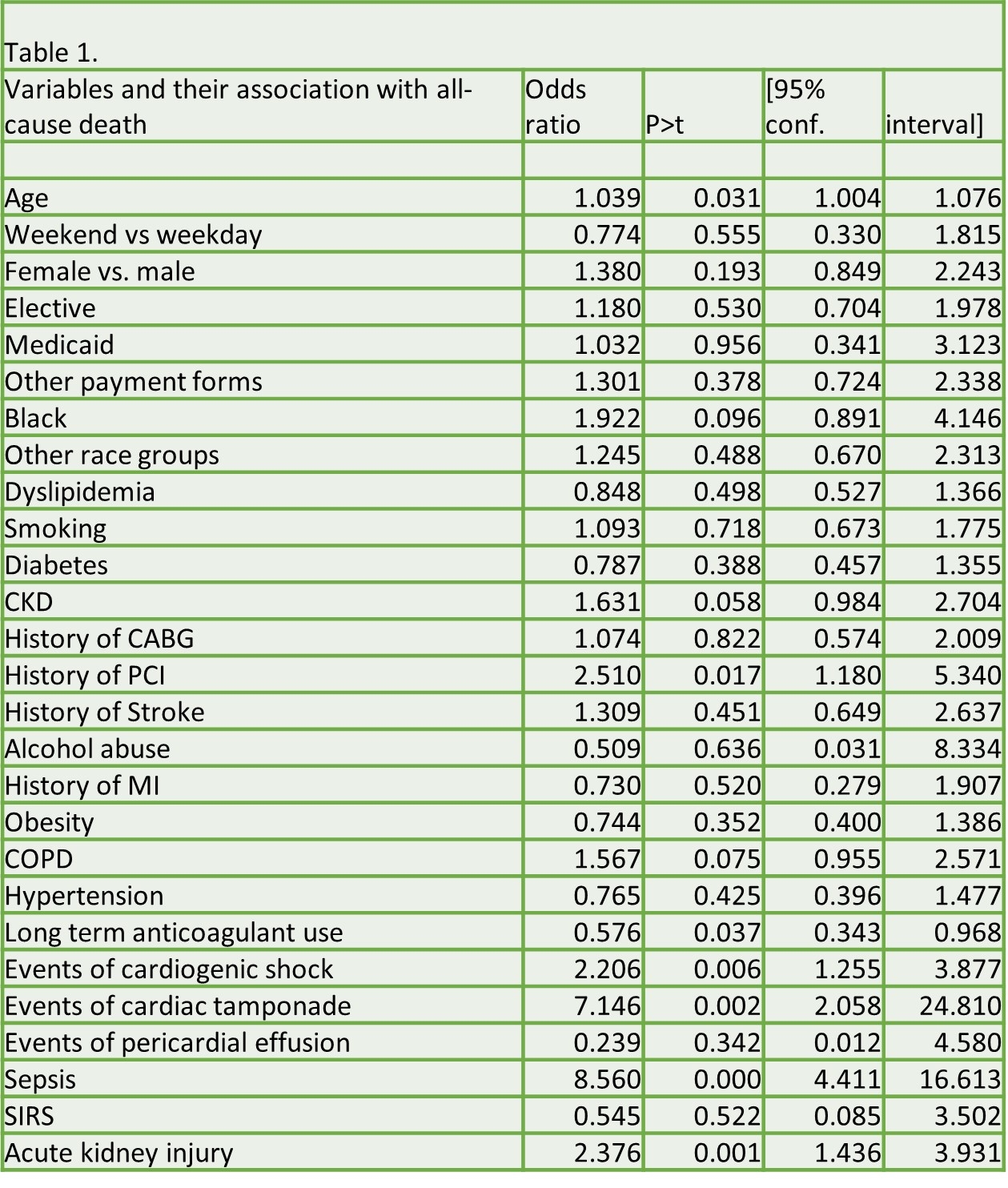
Results: Our study included a total of 6,825 cases of redo surgical mitral valve replacement (redo-SMVR). The overall mortality rate was 7.91% (n=540). Increased mortality was associated with older age, a history of percutaneous coronary intervention (PCI), and long-term anticoagulant use. However, no statistically significant difference in mortality was observed based on weekend (vs. weekday) admission, sex (female vs. male), elective admission status, insurance type (Medicaid/other vs. Medicare), race (Black/other vs. White), or the presence of comorbidities including dyslipidemia, chronic kidney disease (CKD), prior coronary artery bypass grafting (CABG), history of stroke, alcohol abuse, prior myocardial infarction (MI), obesity, chronic obstructive pulmonary disease (COPD), or hypertension. Patients who developed post-procedural complications such as cardiogenic shock, cardiac tamponade, sepsis, and acute kidney injury (AKI) had significantly higher mortality. However, patients with SIRS and pericardial effusion were not statistically associated with increased mortality(Table 1).
Conclusions: Our findings confirm the crucial role that various patient demographics and in-hospital complications have in the all-cause mortality of elderly patients undergoing redo-SMVR. Modifications in treatment protocols and pre- and peri-surgical care should be considered.
Methods: For this study, we considered patients aged 60 years or older who were hospitalized with a primary code for redo-SMVR through the National Inpatient Sample (NIS, 2016-2022). We adopted the methodologies set in prior studies and applied appropriate stratification and clustering of data. The all-cause mortality rates were estimated, and regression models were set up to estimate the adjusted odds ratio (aOR), 95% confidence intervals (95% CI), and p-values of clinically relevant variables.
Results: Our study included a total of 6,825 cases of redo surgical mitral valve replacement (redo-SMVR). The overall mortality rate was 7.91% (n=540). Increased mortality was associated with older age, a history of percutaneous coronary intervention (PCI), and long-term anticoagulant use. However, no statistically significant difference in mortality was observed based on weekend (vs. weekday) admission, sex (female vs. male), elective admission status, insurance type (Medicaid/other vs. Medicare), race (Black/other vs. White), or the presence of comorbidities including dyslipidemia, chronic kidney disease (CKD), prior coronary artery bypass grafting (CABG), history of stroke, alcohol abuse, prior myocardial infarction (MI), obesity, chronic obstructive pulmonary disease (COPD), or hypertension. Patients who developed post-procedural complications such as cardiogenic shock, cardiac tamponade, sepsis, and acute kidney injury (AKI) had significantly higher mortality. However, patients with SIRS and pericardial effusion were not statistically associated with increased mortality(Table 1).
Conclusions: Our findings confirm the crucial role that various patient demographics and in-hospital complications have in the all-cause mortality of elderly patients undergoing redo-SMVR. Modifications in treatment protocols and pre- and peri-surgical care should be considered.
More abstracts on this topic:
Accelerometer-Measured Sedentary Behavior and Future Cardiovascular Disease
Ajufo Ezimamaka, Kany Shinwan, Ramo Joel, Churchill Timothy, Guseh James, Aragam Krishna, Ellinor Patrick, Khurshid Shaan
A Deep Learning Digital Biomarker for Mitral Valve Prolapse using Echocardiogram VideosAl-alusi Mostafa, Khurshid Shaan, Sanborn Danita, Picard Michael, Ho Jennifer, Maddah Mahnaz, Ellinor Patrick, Lau Emily, Small Aeron, Reeder Christopher, Shnitzer Dery Tal, Andrews Carl, Kany Shinwan, Ramo Joel, Haimovich Julian