Final ID: 4369749
Electronegative Lipoprotein Subfractions Modulate Inflammation and Viability in Monocytes and Endothelial cells
Abstract Body (Do not enter title and authors here): Background
Emerging evidence indicates that lipoprotein quality, more than quantity, drives atherogenesis. Lipoproteins can be classified into five subfractions by electronegativity, with subfraction 1 being protective and subfraction 5 the most electronegative and atherogenic. In this study, we examined how the most electronegative subfractions, L5, H5, their combination L5+H5, and total Lp5 (all possible electronegative lipoprotein subtypes; VLDL, IDL, LDL, and HDL) affect cell viability and cytokine production in bovine aortic endothelial cells (BAECs) and THP-1 monocytes.
Objective
To assess how electronegative lipoprotein subfractions affect viability and cytokine production in endothelial cells and monocytes.
Methods
Lipoproteins were isolated by ultracentrifugation, followed by anion-exchange chromatography to obtain electronegative fractions. Cells were exposed to increasing concentrations of subfractions or their combination for 24 hours. Viability was assessed by fluorescence assay after trypan blue exclusion, quantified via image cytometry. Cytokine levels in culture media and cell supernatant were measured by ELISA.
Results
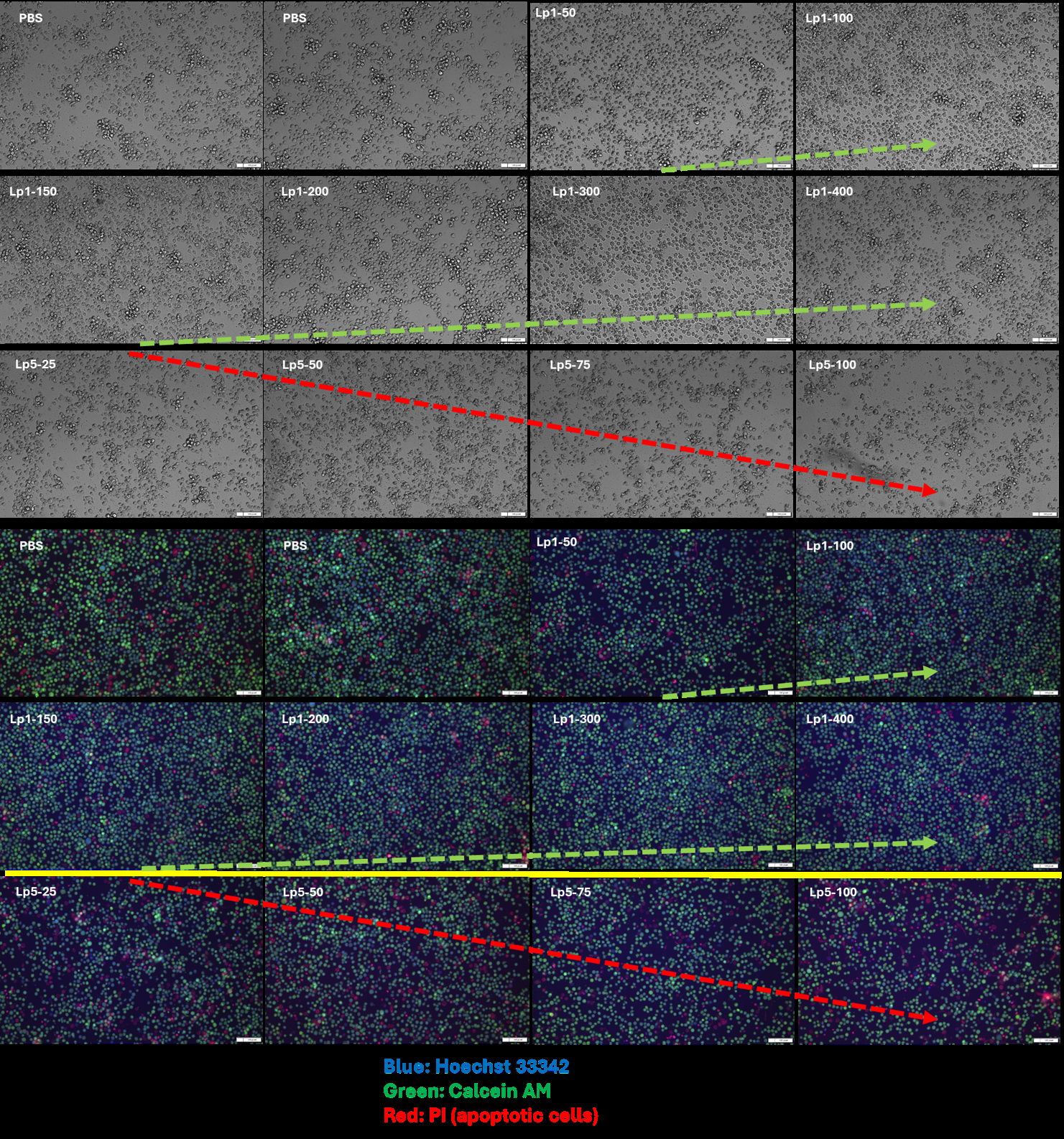
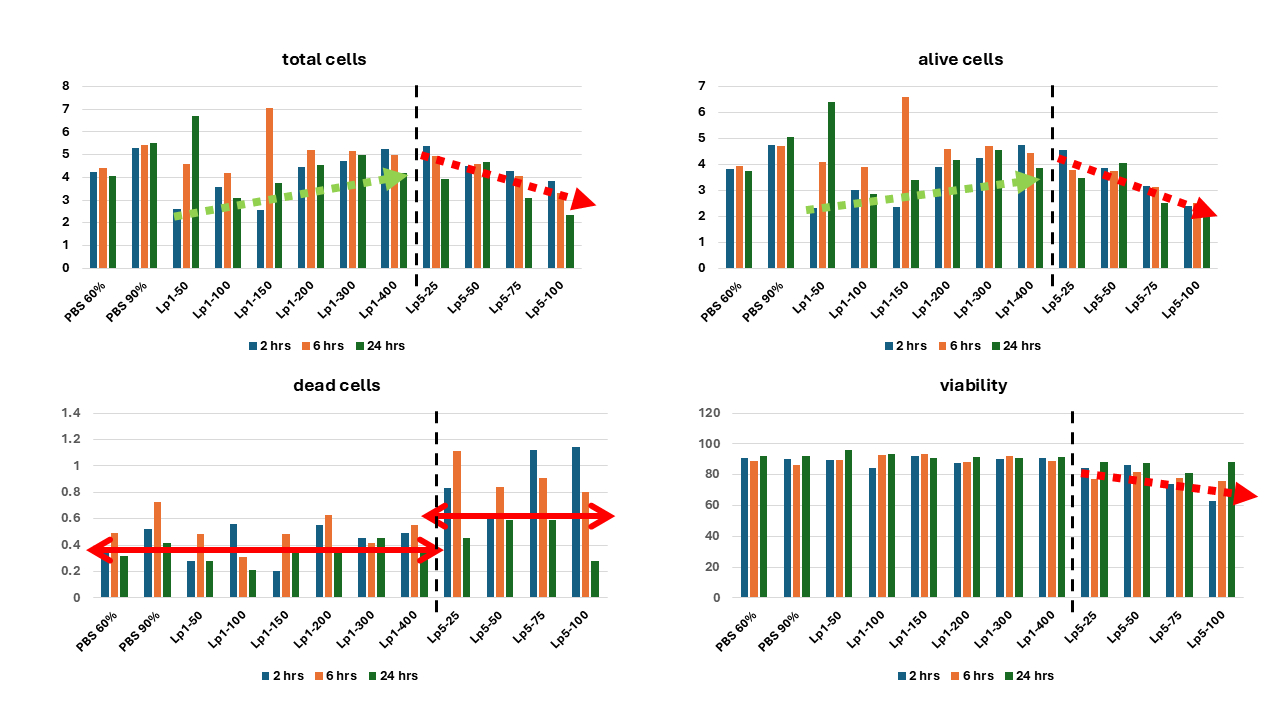
Following 24-hour incubation with single and combined lipoprotein subfractions, varying degrees of changes were observed in IL-6, TNF-α, and IL-10 levels in both cell culture media and cell lysate supernatants of THP-1 and BAEC. Subfraction 5 notably elevated pro-inflammatory cytokines. H5 slightly reduced THP-1 viability, while L5 caused a moderate decrease at 50µg/mL. Their combination produced a synergistic effect, significantly lowering cell number and viability. Total lipoproteins showed the strongest cytotoxicity, with Lp5 exhibiting dose- and time-dependent toxicity (25-100µg/mL) toward THP-1 cells, unlike the less electronegative Lp1 (Fig. 1&2).
Conclusion
Electronegative lipoprotein subfractions reduce endothelial and monocyte viability, indicating cytotoxicity that impairs vascular defenses and promotes atherogenesis. In contrast, the least electronegative subfractions enhance proliferation, suggesting a non-toxic, supportive role. Distinct cytokine profiles highlight divergent immunomodulatory effects and implicate dysfunctional lipoproteins in vascular inflammation and atherosclerosis. These findings highlight the potential clinical relevance of lipoprotein electronegativity, supporting the introduction of a 'lipoprotein electronegativity index' as a novel marker for assessing lipoprotein quality and atherogenic risk.
Emerging evidence indicates that lipoprotein quality, more than quantity, drives atherogenesis. Lipoproteins can be classified into five subfractions by electronegativity, with subfraction 1 being protective and subfraction 5 the most electronegative and atherogenic. In this study, we examined how the most electronegative subfractions, L5, H5, their combination L5+H5, and total Lp5 (all possible electronegative lipoprotein subtypes; VLDL, IDL, LDL, and HDL) affect cell viability and cytokine production in bovine aortic endothelial cells (BAECs) and THP-1 monocytes.
Objective
To assess how electronegative lipoprotein subfractions affect viability and cytokine production in endothelial cells and monocytes.
Methods
Lipoproteins were isolated by ultracentrifugation, followed by anion-exchange chromatography to obtain electronegative fractions. Cells were exposed to increasing concentrations of subfractions or their combination for 24 hours. Viability was assessed by fluorescence assay after trypan blue exclusion, quantified via image cytometry. Cytokine levels in culture media and cell supernatant were measured by ELISA.
Results
Following 24-hour incubation with single and combined lipoprotein subfractions, varying degrees of changes were observed in IL-6, TNF-α, and IL-10 levels in both cell culture media and cell lysate supernatants of THP-1 and BAEC. Subfraction 5 notably elevated pro-inflammatory cytokines. H5 slightly reduced THP-1 viability, while L5 caused a moderate decrease at 50µg/mL. Their combination produced a synergistic effect, significantly lowering cell number and viability. Total lipoproteins showed the strongest cytotoxicity, with Lp5 exhibiting dose- and time-dependent toxicity (25-100µg/mL) toward THP-1 cells, unlike the less electronegative Lp1 (Fig. 1&2).
Conclusion
Electronegative lipoprotein subfractions reduce endothelial and monocyte viability, indicating cytotoxicity that impairs vascular defenses and promotes atherogenesis. In contrast, the least electronegative subfractions enhance proliferation, suggesting a non-toxic, supportive role. Distinct cytokine profiles highlight divergent immunomodulatory effects and implicate dysfunctional lipoproteins in vascular inflammation and atherosclerosis. These findings highlight the potential clinical relevance of lipoprotein electronegativity, supporting the introduction of a 'lipoprotein electronegativity index' as a novel marker for assessing lipoprotein quality and atherogenic risk.
More abstracts on this topic:
A20 in the Kidney Epithelium Attenuates Angiotensin II-induced Hypertension by Constraining Renal Tubular NHE3 Expression
Lu Xiaohan, Ren Jiafa, Wen Yi, Griffiths Robert, Yang Ting, Hammer Gianna, Zhuo Jia, Crowley Steven
Association of Elevated Serum Lipoprotein(a) with New-Onset Atrial Fibrillation: A Retrospective Study of 108930 PatientsKamel Moaz, Arsanjani Reza, Awad Kamal, Mahmoud Ahmed K., Farina Juan, Scalia Isabel, Pereyra Milagros, Abbas Mohammed Tiseer, Baba Nima, Ayoub Chadi