Final ID: MP484
Where Cardiac Arrest Claims: A Mapping of End-of-Life Care by Demographics and Region, 1999–2024
Abstract Body (Do not enter title and authors here): Introduction/Background:
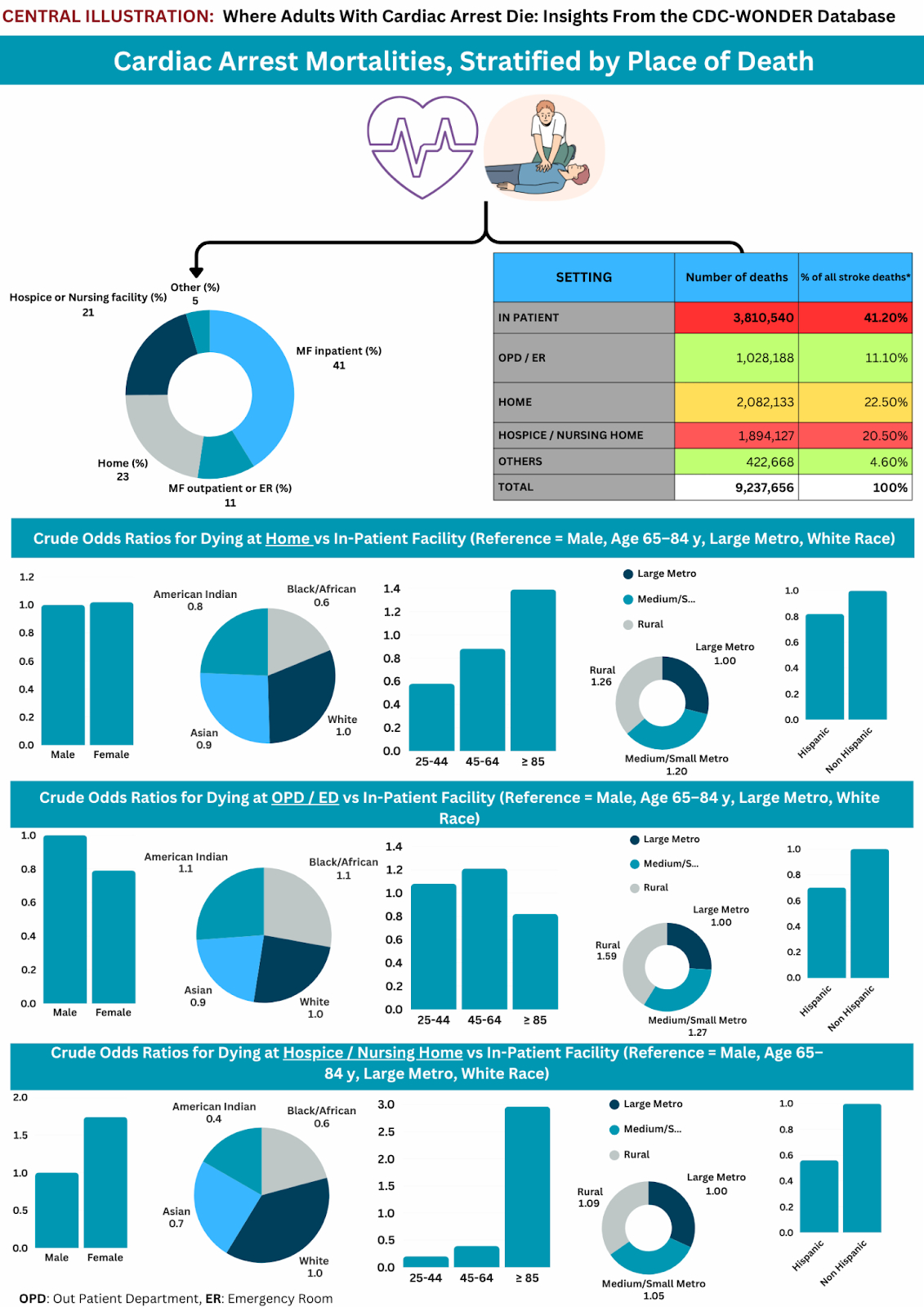
Cardiac arrest caused >9M U.S. adult deaths (1999–2024). Place of death reflects end-of-life care quality. While home/hospice deaths rose for other conditions, cardiac arrest patterns by demographics remain understudied.
Research Questions/Hypothesis:
Death location varies by demographics, with younger/minority patients more likely to die in EDs and less likely in hospice than older White patients.
Methods/Approach:
From CDC WONDER, we extracted all U.S. adult (≥25 y) deaths attributed to cardiac arrest (ICD-10 I46) from 1999–2021. Place of death was categorized as inpatient (ref), ED/outpatient, home, hospice/nursing, or other. Crude ORs (95% CIs) comparing each non-inpatient location to inpatient were computed via 2×2 tables, stratified by age (25–44, 45–64, 65–84 [ref], ≥85), sex (male [ref], female), race (White [ref], Black, AI/PI), Hispanic origin (non-Hispanic [ref], Hispanic), and urbanization (large metro [ref], medium/small metro, rural
Results/Data:
Overall, 41.2% died in hospital; 11.1% in outpatient/ED; 22.5% at home; 20.5% in hospice/nursing; 4.6% elsewhere. Compared with 65–84, 25–44 showed lower home (OR 0.58; 95% CI 0.57–0.58; P<0.001) and hospice (OR 0.20; 95% CI 0.18–0.22; P<0.001), but higher ED (OR 1.08; 95% CI 1.07–1.09; P<0.001). Conversely, ≥85 had higher home (OR 1.39; 95% CI 1.38–1.39; P<0.001) and hospice (OR 2.96; 95% CI 2.95–2.97; P<0.001), but lower ED (OR 0.82; 95% CI 0.81–0.82; P<0.001). Females had higher home (OR 1.02; 95% CI 1.02–1.03; P<0.001) and hospice (OR 1.74; 95% CI 1.73–1.74; P<0.001), but lower ED (OR 0.79; 95% CI 0.79–0.80; P<0.001). Blacks had lower home (OR 0.61; 95% CI 0.61–0.62; P<0.001) and hospice (OR 0.55; 95% CI 0.55–0.55; P<0.001), but higher ED (OR 1.13; 95% CI 1.12–1.14; P<0.001) versus Whites. Hispanics had lower home (OR 0.82; 95% CI 0.82–0.83; P<0.001), ED (OR 0.69; 95% CI 0.69–0.70; P<0.001), and hospice (OR 0.56; 95% CI 0.56–0.56; P<0.001) than non-Hispanics. Rural decedents had higher home (OR 1.26; 95% CI 1.25–1.26; P<0.001), ED (OR 1.59; 95% CI 1.58–1.60; P<0.001), and hospice (OR 1.09; 95% CI 1.09–1.10; P<0.001) versus large-metro.
Conclusion(s):
Only 41% died in hospital. Young adults had higher ED deaths; ≥ 85 and women had more home/hospice deaths. Blacks, Hispanics, and rural groups faced lower home/hospice and higher ED mortality, warranting equitable palliative care interventions.
Cardiac arrest caused >9M U.S. adult deaths (1999–2024). Place of death reflects end-of-life care quality. While home/hospice deaths rose for other conditions, cardiac arrest patterns by demographics remain understudied.
Research Questions/Hypothesis:
Death location varies by demographics, with younger/minority patients more likely to die in EDs and less likely in hospice than older White patients.
Methods/Approach:
From CDC WONDER, we extracted all U.S. adult (≥25 y) deaths attributed to cardiac arrest (ICD-10 I46) from 1999–2021. Place of death was categorized as inpatient (ref), ED/outpatient, home, hospice/nursing, or other. Crude ORs (95% CIs) comparing each non-inpatient location to inpatient were computed via 2×2 tables, stratified by age (25–44, 45–64, 65–84 [ref], ≥85), sex (male [ref], female), race (White [ref], Black, AI/PI), Hispanic origin (non-Hispanic [ref], Hispanic), and urbanization (large metro [ref], medium/small metro, rural
Results/Data:
Overall, 41.2% died in hospital; 11.1% in outpatient/ED; 22.5% at home; 20.5% in hospice/nursing; 4.6% elsewhere. Compared with 65–84, 25–44 showed lower home (OR 0.58; 95% CI 0.57–0.58; P<0.001) and hospice (OR 0.20; 95% CI 0.18–0.22; P<0.001), but higher ED (OR 1.08; 95% CI 1.07–1.09; P<0.001). Conversely, ≥85 had higher home (OR 1.39; 95% CI 1.38–1.39; P<0.001) and hospice (OR 2.96; 95% CI 2.95–2.97; P<0.001), but lower ED (OR 0.82; 95% CI 0.81–0.82; P<0.001). Females had higher home (OR 1.02; 95% CI 1.02–1.03; P<0.001) and hospice (OR 1.74; 95% CI 1.73–1.74; P<0.001), but lower ED (OR 0.79; 95% CI 0.79–0.80; P<0.001). Blacks had lower home (OR 0.61; 95% CI 0.61–0.62; P<0.001) and hospice (OR 0.55; 95% CI 0.55–0.55; P<0.001), but higher ED (OR 1.13; 95% CI 1.12–1.14; P<0.001) versus Whites. Hispanics had lower home (OR 0.82; 95% CI 0.82–0.83; P<0.001), ED (OR 0.69; 95% CI 0.69–0.70; P<0.001), and hospice (OR 0.56; 95% CI 0.56–0.56; P<0.001) than non-Hispanics. Rural decedents had higher home (OR 1.26; 95% CI 1.25–1.26; P<0.001), ED (OR 1.59; 95% CI 1.58–1.60; P<0.001), and hospice (OR 1.09; 95% CI 1.09–1.10; P<0.001) versus large-metro.
Conclusion(s):
Only 41% died in hospital. Young adults had higher ED deaths; ≥ 85 and women had more home/hospice deaths. Blacks, Hispanics, and rural groups faced lower home/hospice and higher ED mortality, warranting equitable palliative care interventions.
More abstracts on this topic:
A Meta-Analysis on the Effect of Chronic Total Occlusion of Coronary Arteries on Cardiovascular Outcomes in Patients Undergoing Transcatheter Aortic Valve Replacement
Goyal Aman, Tariq Muhammad Daoud, Zahra Rubab, Jain Hritvik, Khan Rozi, Mahalwar Gauranga
Accelerometer-Measured Sedentary Behavior and Future Cardiovascular DiseaseAjufo Ezimamaka, Kany Shinwan, Ramo Joel, Churchill Timothy, Guseh James, Aragam Krishna, Ellinor Patrick, Khurshid Shaan