Final ID: MP740
Between Risk and Return: Predicting Gaps In Care For Those With Congenital Heart Disease Through Machine Learning and Social Risk Modeling
Abstract Body (Do not enter title and authors here): Introduction/ Background:
Lifelong continuity of care is essential for individuals with congenital heart disease (CHD). Despite guidelines recommending uninterrupted follow-up, gaps in care (GIC) remain common and are associated with adverse health outcomes. The underlying factors contributing to GIC are not well understood. Machine learning offers a novel approach to identify at-risk populations and understand predictors of GIC.
Research Questions/Hypothesis:
We aimed to develop and evaluate a machine learning model to predict which CHD patients are most at risk for GIC and to identify key social determinants of health demographics and clinical features contributing to GIC.
Methods /Approach:
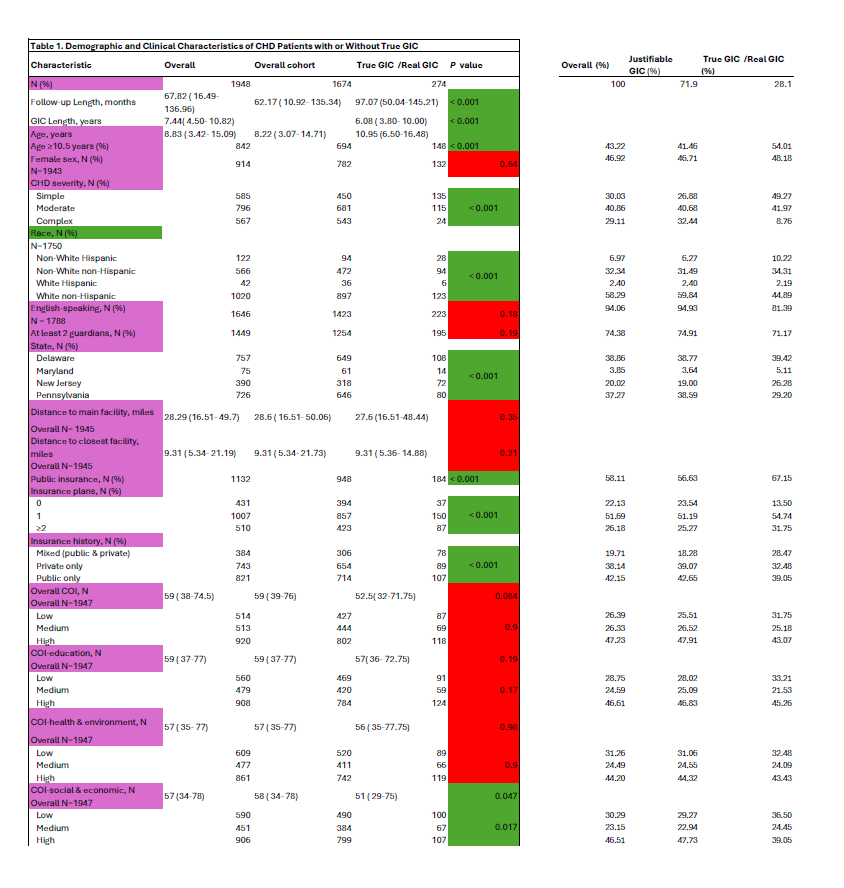
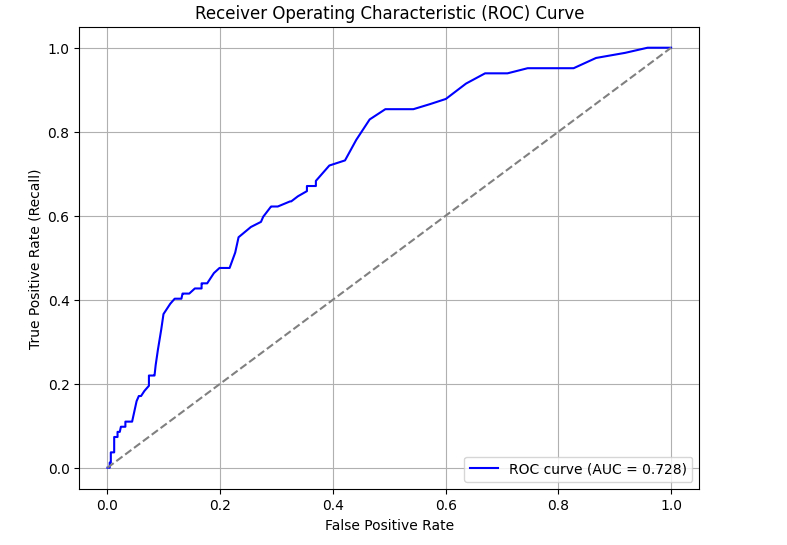
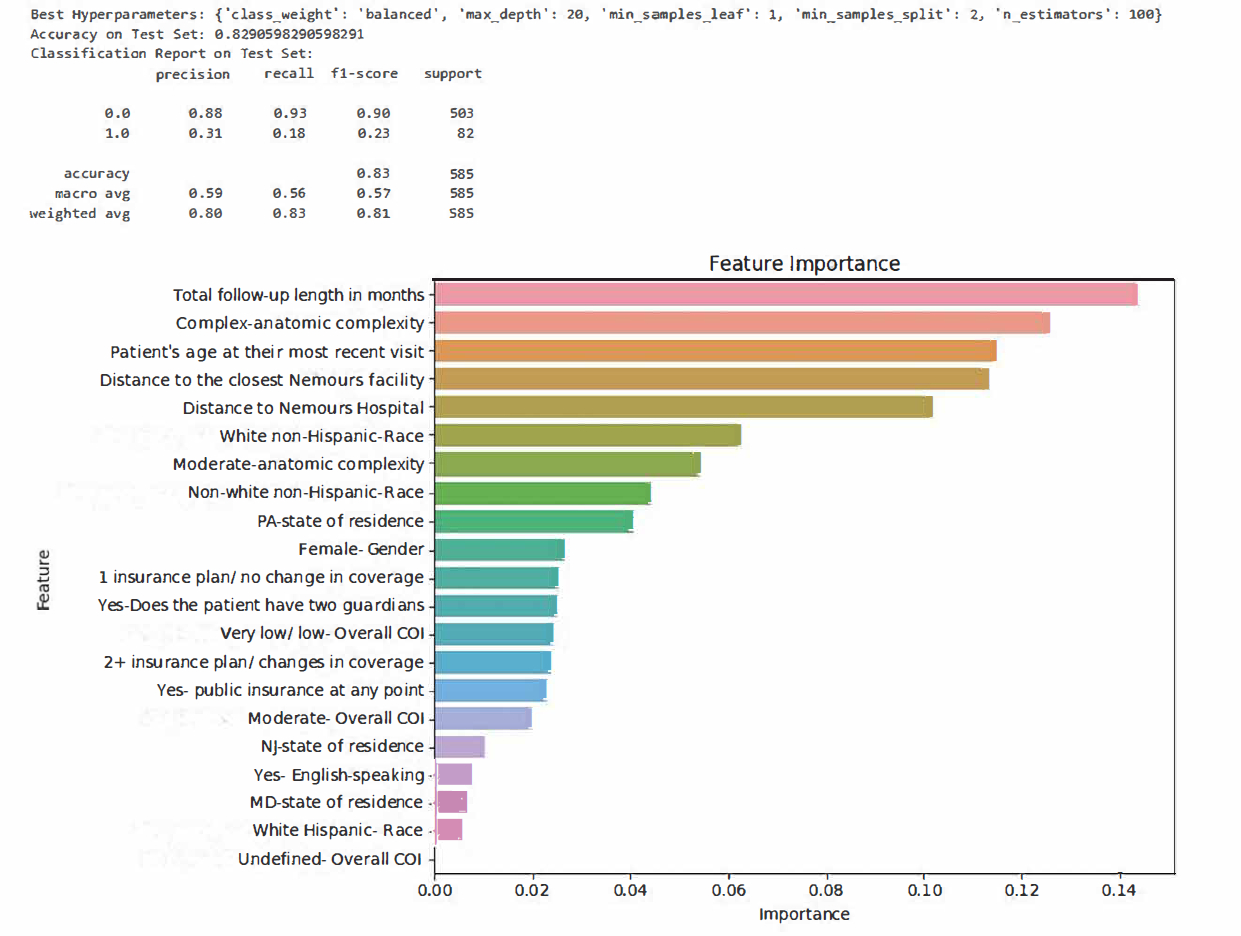
In this retrospective cohort study, we analyzed 1,948 CHD patients aged 0–34 years who underwent surgery at a multi-state pediatric subspecialty center from 2003-2020. A GIC was defined as a >3 year lapse between cardiology visits. Patients were categorized as GIC (n=274) or without GIC (n=1674). Demographics and SDOH, including race, ethnicity, sex, language, and Child Opportunity Index (COI) by ZIP code, were incorporated into the model. A Random Forest classifier was trained on a 70:30 split dataset using Synthetic Minority Over-sampling Technique to address class imbalance. Model optimization involved hyperparameter tuning via GridSearchCV and was evaluated using ROC, feature importance, and F1 score.
Results/Data:
The model demonstrated good overall performance, with an AUC of 0.728. Among patients without GIC, the model showed strong precision (0.88), recall (0.93), and F1 score (0.90), highlighting its ability to correctly identify those maintaining follow-up. While performance was more limited in predicting GIC (F1 score: 0.23), the model provides a foundational step toward improving predictive accuracy in this group. Key features influencing follow-up status included time since last visit, anatomic complexity, age >10.5 years, greater distance to care, and white non-Hispanic race/ethnicity (Figures 1–3).
Conclusion:
This study highlights the potential of machine learning to proactively identify CHD patients at risk for GIC. Though additional training is needed to optimize predictions for the GIC group, current findings demonstrate moderate to high accuracy in identifying patients who maintain care. These insights can inform targeted strategies based on clinical and social risk factors to reduce GIC and improve long-term outcomes.
Lifelong continuity of care is essential for individuals with congenital heart disease (CHD). Despite guidelines recommending uninterrupted follow-up, gaps in care (GIC) remain common and are associated with adverse health outcomes. The underlying factors contributing to GIC are not well understood. Machine learning offers a novel approach to identify at-risk populations and understand predictors of GIC.
Research Questions/Hypothesis:
We aimed to develop and evaluate a machine learning model to predict which CHD patients are most at risk for GIC and to identify key social determinants of health demographics and clinical features contributing to GIC.
Methods /Approach:
In this retrospective cohort study, we analyzed 1,948 CHD patients aged 0–34 years who underwent surgery at a multi-state pediatric subspecialty center from 2003-2020. A GIC was defined as a >3 year lapse between cardiology visits. Patients were categorized as GIC (n=274) or without GIC (n=1674). Demographics and SDOH, including race, ethnicity, sex, language, and Child Opportunity Index (COI) by ZIP code, were incorporated into the model. A Random Forest classifier was trained on a 70:30 split dataset using Synthetic Minority Over-sampling Technique to address class imbalance. Model optimization involved hyperparameter tuning via GridSearchCV and was evaluated using ROC, feature importance, and F1 score.
Results/Data:
The model demonstrated good overall performance, with an AUC of 0.728. Among patients without GIC, the model showed strong precision (0.88), recall (0.93), and F1 score (0.90), highlighting its ability to correctly identify those maintaining follow-up. While performance was more limited in predicting GIC (F1 score: 0.23), the model provides a foundational step toward improving predictive accuracy in this group. Key features influencing follow-up status included time since last visit, anatomic complexity, age >10.5 years, greater distance to care, and white non-Hispanic race/ethnicity (Figures 1–3).
Conclusion:
This study highlights the potential of machine learning to proactively identify CHD patients at risk for GIC. Though additional training is needed to optimize predictions for the GIC group, current findings demonstrate moderate to high accuracy in identifying patients who maintain care. These insights can inform targeted strategies based on clinical and social risk factors to reduce GIC and improve long-term outcomes.
More abstracts on this topic:
Anatomic Physiological Scoring is a Comparable Predictor of Adult Congenital Operative Morbidity and Mortality
La Brenda, Taylor-fishwick Jon, Macbeth Morgan, Soohoo Megan
A machine learning approach to examining the associations of minority stressors and physical activity among sexual and gender minority adultsLopez Veneros David, Ensari Ipek, Bhilegaonkar Riya, Sharma Yashika, Caceres Billy