Final ID: MP1571
Risk of Arrhythmia Persists Throughout Acute and Chronic Phases of Autonomic Dysreflexia following Spinal Cord Injury: A Rodent Model Study
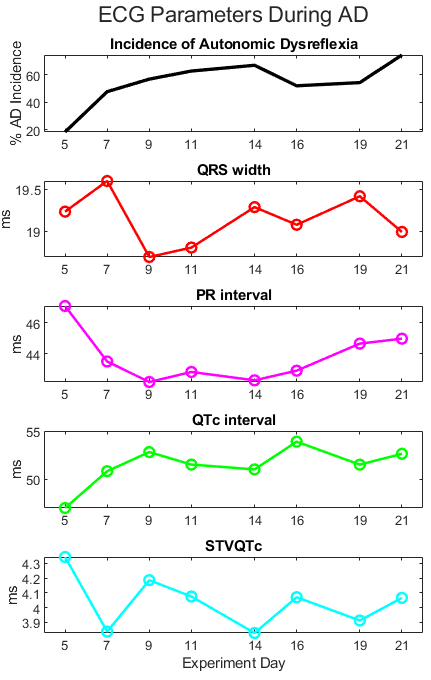
Abstract Body (Do not enter title and authors here): Autonomic Dysreflexia (AD) is a potentially life-threatening overreaction of the sympathetic nervous system that commonly occurs in individuals with spinal cord injuries at or above the T6 level. This uncoordinated response to noxious stimuli below the level of injury triggers episodes of severe hypertension that persist until the stimulus is removed. Although arrhythmias such as atrial fibrillation have been identified as complications of AD, little is known about the long-term risk of arrhythmia across both the acute and chronic phases of AD. To model AD, ten Sprague-Dawley rats underwent spinal cord compression injury at the T3 level. For each animal, three trials of colorectal distension (CRD) were conducted to induce AD on days 5, 7, 9, 11, 14, 16, 19, and 21 post-injury. Implanted radio telemetry devices and surface electrodes collected blood pressure and electrocardiogram (ECG) signals. Trials were classified as AD if systolic blood pressure increased by ≥ 15 mmHg relative to baseline. ECG parameters were analyzed to assess arrhythmia risk. During AD, there was a significantly shortened PR interval (p = 0.00286), decreased QRS width (p < 0.001), decreased corrected QT (QTc) interval (p <0.001), and increased short-term variability of the QTc (STVQTc) (p < 0.001). No significant changes in RR interval were observed. Baseline STVQTc was significantly higher during the chronic phase (days 14-21) compared to the acute phase (days 5-11) (p = 0.0107). Arrhythmias such as premature ventricular contractions (PVC) and atrial flutter were observed in seven of ten rats. Temporal analysis revealed the same significant changes in ECG parameters during AD across the study period. Notably, increased baseline STVQTc during the chronic phase suggests elevated vulnerability even outside of active AD. Additionally, ECG parameter trends mirror AD incidence. Trends shift around day 14, marking the onset of the chronic phase of AD (see figure). Risk of arrhythmia associated with AD is not limited to hypertensive episodes but reflects persistent vulnerability over time. Because RR intervals remained unchanged, the observed ECG fluctuations are unlikely due to heart rate and instead indicate the potential contribution of AD to altered cardiac electrophysiology. As ECG dynamics reflect the trajectory of AD incidence, future investigations should explore the mechanisms linking sympathetic overreaction and cardiac electrophysiology.
More abstracts on this topic:
A major effect of aprocitentan on albuminuria in patients with resistant hypertension
Schlaich Markus, Bakris George, Flack John, Gimona Alberto, Narkiewicz Krzysztof, Sassi-sayadi Mouna, Wang Jiguang, Weber Michael
A New Biomarker of Aging Derived From Electrocardiogram Improves Risk Prediction of Incident Myocardial Infarction and Stroke.Wilsgaard Tom, Rosamond Wayne, Schirmer Henrik, Lindekleiv Haakon, Attia Zachi, Lopez-jimenez Francisco, Leon David, Iakunchykova Olena