Final ID: MP2432
Demographic and Regional Disparities in Mortality due to Congenital Heart Diseases Among Adults in the United States: Insight from a 24-Year Retrospective Analysis
Abstract Body (Do not enter title and authors here): Background
Advances in care have significantly improved survival for those with congenital heart disease (CHD), creating a growing adult CHD population. However, a limited number of studies on this topic emphasizes the need for deeper exploration of mortality trends among these adults.
Aims
The purpose of this study was to assess demographic and regional disparities in mortality trends among adults with CHD in the United States.
Methods
Death certificates from the CDC WONDER (Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research) database were examined from 1999 to 2023 for congenital heart diseases related mortality in adults ≥25 years of age. Age-adjusted mortality rates (AAMRs) per 100,000 persons and annual percent change (APC) were calculated and stratified by year, age, sex, race/ethnicity, place of death, urbanisation and geographic region.
Results
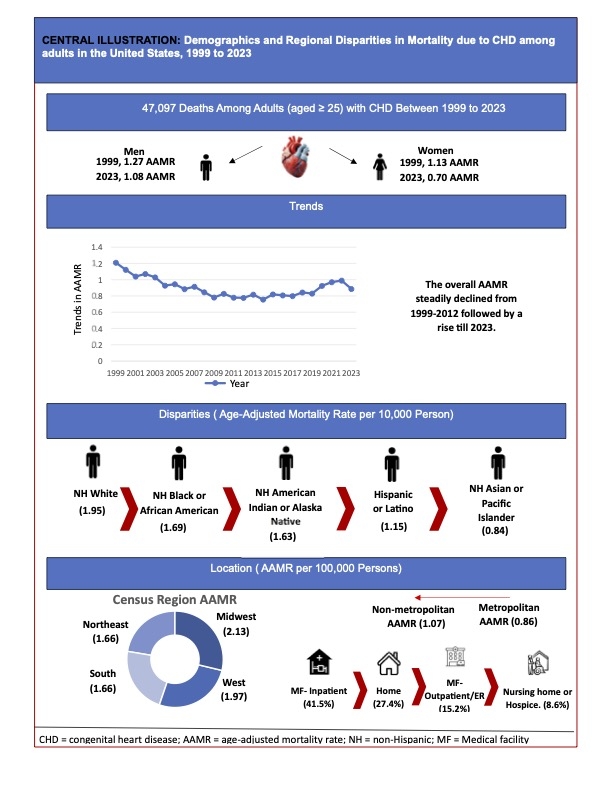
Between 1999 and 2023, 47,097 deaths occurred among adults aged ≥25 years. The AAMR declined from 1.20 in 1999 to 0.78 in 2012 (APC: -3.26; 95% CI: -3.9 to -2.6), after which it significantly increased to 0.88 in 2023 (APC: 2.21; 95% CI: 1.3 to 3.1). Males consistently exhibited higher AAMR compared to females from 1999 (AAMR men: 1.27 vs women: 1.13) to 2023 (AAMR men: 1.08 vs women: 0.70). Non-Hispanic (NH) White adults had the highest overall AAMR (1.95), followed by NH Black (1.69), NH American Indian/Alaska Native (1.63), Hispanic or Latino (1.15), and NH Asian or Pacific Islander adults (0.84). Regional differences were observed, with the Midwest reporting the highest AAMR (2.13), followed by the West (1.97), Northeast (1.66), and South (1.66). Mortality rates were higher in nonmetropolitan areas (1.07) compared to metropolitan areas (0.86). Most deaths occurred in inpatient medical facilities (41.5%), followed by home (27.4%), outpatient/emergency departments (15.2%), and hospice/nursing facilities (8.6%). Crude mortality rates (CMRs) increased with age, peaking in adults aged ≥85 years (7.11 per 100,000), and declined progressively across younger 10-year age groups to the lowest rate in those aged 25–34 years (1.19).
Conclusion
AAMR due to congenital heart disease in U.S. adults initially declined from 1999 to 2012 but they have risen since 2012, indicating a reversal of prior gains. Persistent demographic and geographic disparities in CHD mortality highlight the need for further investigation and targeted interventions to address inequities in outcomes.
Advances in care have significantly improved survival for those with congenital heart disease (CHD), creating a growing adult CHD population. However, a limited number of studies on this topic emphasizes the need for deeper exploration of mortality trends among these adults.
Aims
The purpose of this study was to assess demographic and regional disparities in mortality trends among adults with CHD in the United States.
Methods
Death certificates from the CDC WONDER (Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research) database were examined from 1999 to 2023 for congenital heart diseases related mortality in adults ≥25 years of age. Age-adjusted mortality rates (AAMRs) per 100,000 persons and annual percent change (APC) were calculated and stratified by year, age, sex, race/ethnicity, place of death, urbanisation and geographic region.
Results
Between 1999 and 2023, 47,097 deaths occurred among adults aged ≥25 years. The AAMR declined from 1.20 in 1999 to 0.78 in 2012 (APC: -3.26; 95% CI: -3.9 to -2.6), after which it significantly increased to 0.88 in 2023 (APC: 2.21; 95% CI: 1.3 to 3.1). Males consistently exhibited higher AAMR compared to females from 1999 (AAMR men: 1.27 vs women: 1.13) to 2023 (AAMR men: 1.08 vs women: 0.70). Non-Hispanic (NH) White adults had the highest overall AAMR (1.95), followed by NH Black (1.69), NH American Indian/Alaska Native (1.63), Hispanic or Latino (1.15), and NH Asian or Pacific Islander adults (0.84). Regional differences were observed, with the Midwest reporting the highest AAMR (2.13), followed by the West (1.97), Northeast (1.66), and South (1.66). Mortality rates were higher in nonmetropolitan areas (1.07) compared to metropolitan areas (0.86). Most deaths occurred in inpatient medical facilities (41.5%), followed by home (27.4%), outpatient/emergency departments (15.2%), and hospice/nursing facilities (8.6%). Crude mortality rates (CMRs) increased with age, peaking in adults aged ≥85 years (7.11 per 100,000), and declined progressively across younger 10-year age groups to the lowest rate in those aged 25–34 years (1.19).
Conclusion
AAMR due to congenital heart disease in U.S. adults initially declined from 1999 to 2012 but they have risen since 2012, indicating a reversal of prior gains. Persistent demographic and geographic disparities in CHD mortality highlight the need for further investigation and targeted interventions to address inequities in outcomes.
More abstracts on this topic:
Abnormal Oxygen Pulse Trajectory Differentiates Anatomic Complexity and Functional Classification in Adults with Congenital Heart Disease
Campbell Matthew, Lefebvre Margaret, Li Pengyang, Padgett Hannah, Tchoukina Inna, Canada Justin, Shah Sangeeta, Rouse Sierra, Reyes Oscar, Shin Yongdeok, Bakken Brad, Coe Alexa, Hallam Jessica, Kapa Meghana
Adult congenital heart disease (ACHD) as career? Examining encouraging and discouraging factors around the globe in the Global ACHD Survey.Bravo-jaimes Katia, Elizari Maria Amalia, Valdez Ramos Miriam, Cupido Blanche, Zentner Dominica, Almasri Murad, Phillips Sabrina, Mcleod Christopher, Burchill Luke, Bullock-palmer Renee, Windram Jonathan, Srour Mhd Osama, Jenkins Petra, Luna-lopez Raquel, Tutarel Oktay, Kandavello Geetha, Guerrero Carlos, García Cruz Edgar, Ackerman Judith