Final ID: MP2161
National Patterns of Use of Electronic Health Record–Integrated Artificial Intelligence Predictive Models at US Hospitals and their Performance on Key Cardiovascular Outcomes
Abstract Body (Do not enter title and authors here): Background: While predictive models that leverage artificial intelligence (AI) have been proposed to improve clinical outcomes, it is essential to examine the current landscape of their dissemination and integration at US hospitals.
Aim: To evaluate the national patterns of use of AI-enabled prediction tools at US hospitals, and their association with hospital features and performance on cardiovascular outcome measures.
Methods: We leveraged the 2023 American Hospital Association (AHA) Annual IT Supplement. This included a national survey of US hospitals querying whether hospitals use EHR-integrated AI predictive models in care processes. We used AHA survey to identify a range of hospital characteristics, and linked the data to the CMS Hospital Quality Reports (2020–2023) to evaluate whether hospitals adopting these technologies represented those leading or lagging in cardiovascular performance measures, including risk-standardized 30-day mortality and readmission rates for acute myocardial infarction (AMI) and heart failure (HF). To assess these relationships, we used multivariable linear regression models adjusting for hospital characteristics.
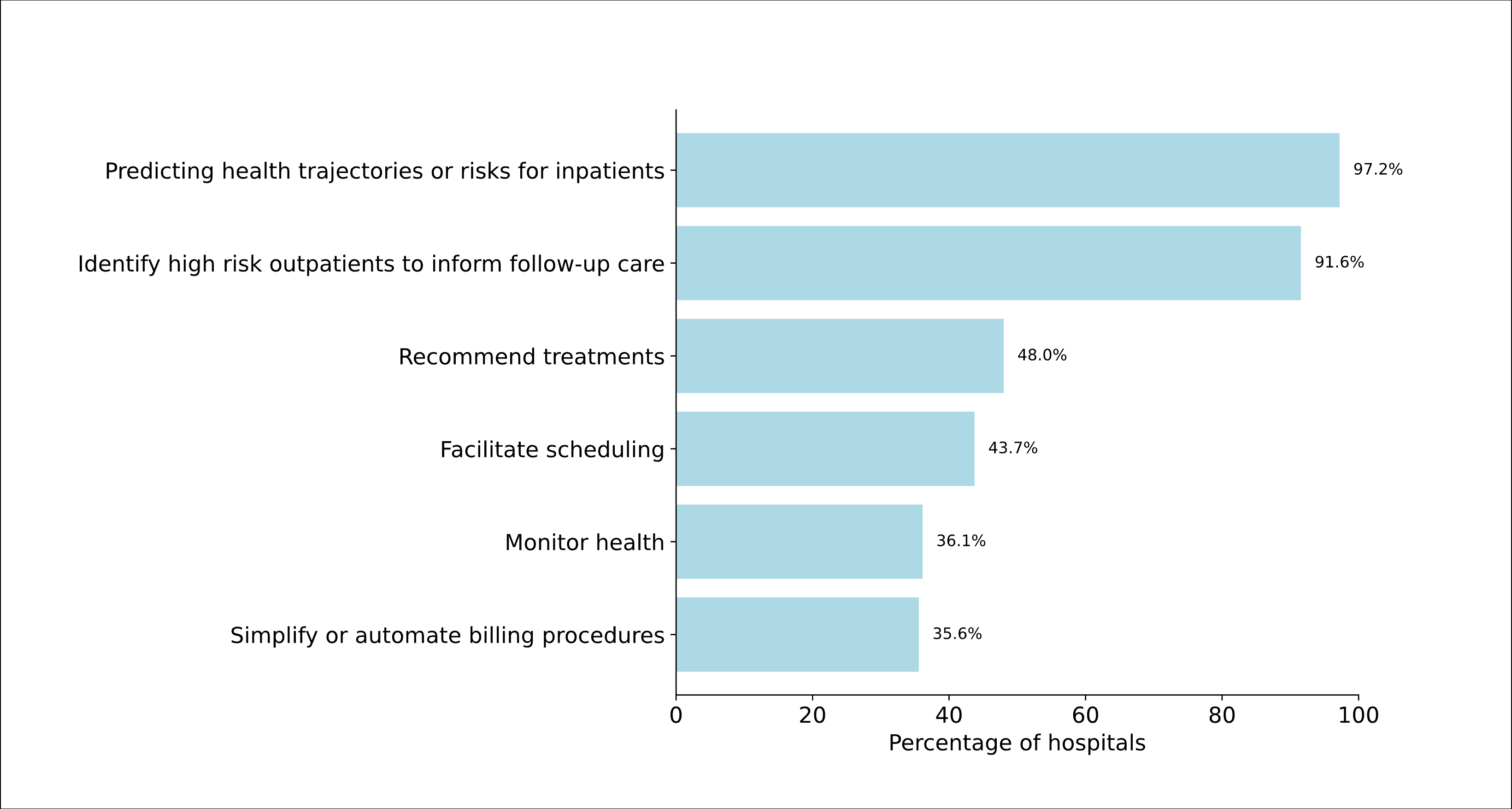
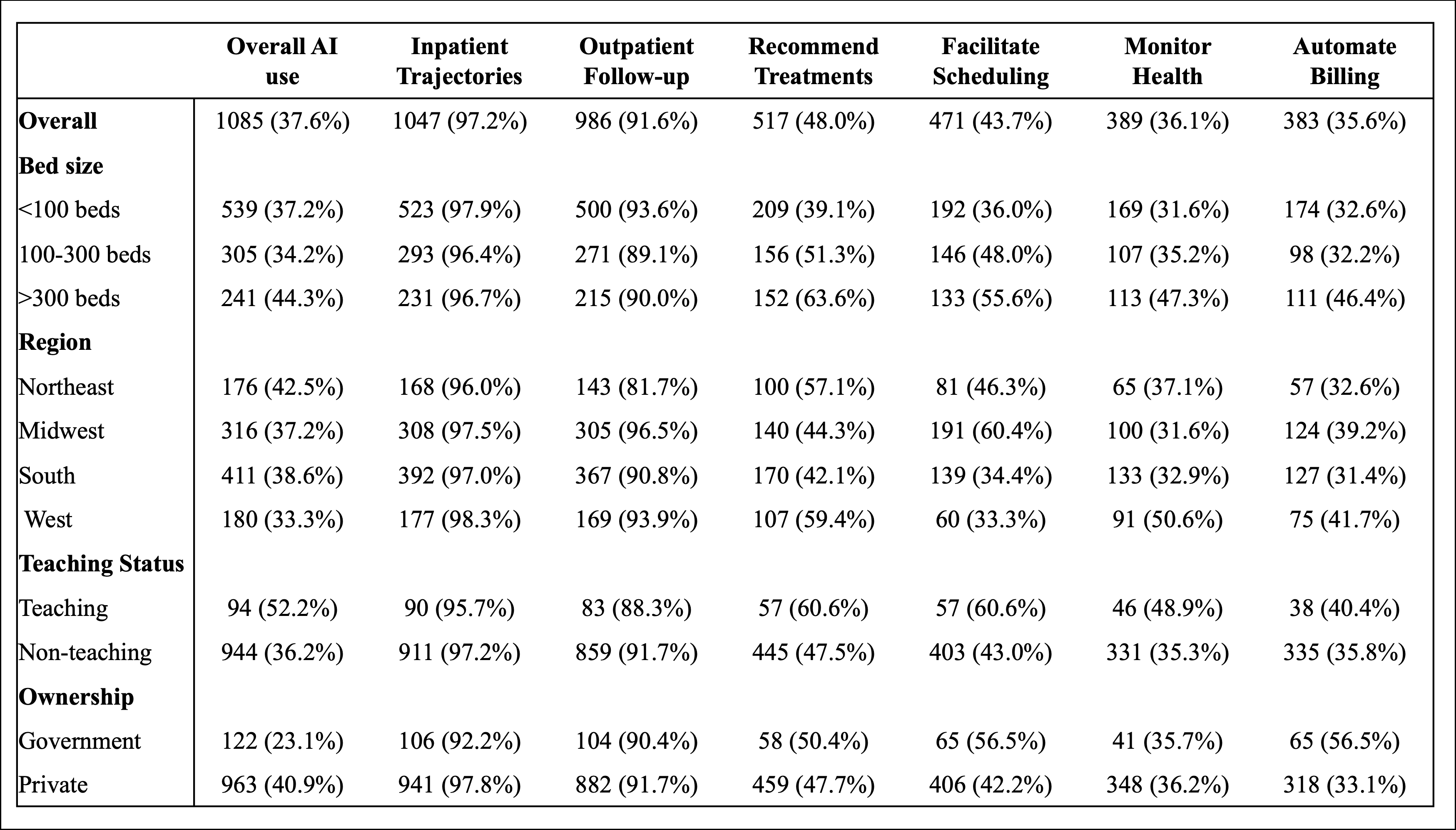
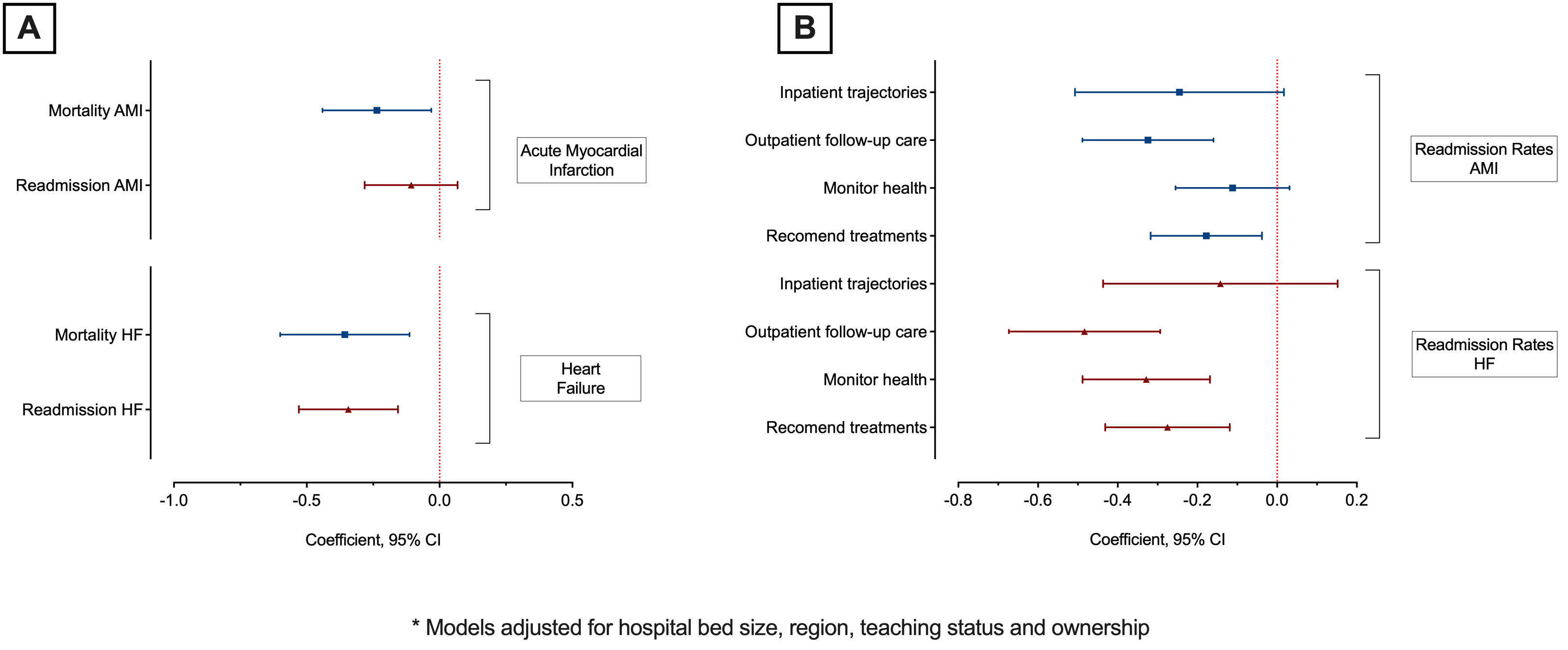
Results: Among 2,885 hospitals in the AHA IT Survey, 1,085 (37.6%) reported using EHR-integrated AI-based predictive models, while 866 reported using only non-AI tools. The most common clinical applications of AI included predicting inpatient health trajectories (97.2%) and identifying high-risk outpatients for follow-up care (91.6%) (Figure 1). AI use was highest among hospitals with bedsize ≥300 (44.3% vs 37.2% in <100 beds), those located in the Northeast (42.5% vs 33.3% in the West), teaching (52.2% vs 36.2% non-teaching), and private hospitals (40.9% vs 23.1% government owned) (Figure 2). Hospitals with integrated AI technology, on average, reported a lower 30-day mortality rate for both AMI and HF, as well as modestly lower readmission rates for HF, but not AMI (Figure 3A). Hospitals reporting use of AI tools specifically for outpatient follow-up and treatment recommendation had lower readmission rates for both AMI and HF (Figure 3B).
Conclusions: Only a 3rd of US hospitals that participated in a national survey about health IT reported the use of EHR-integrated AI tools, with differential uptake across hospitals and use cases. There is a need for a national strategy to integrate and monitor health AI care systematically.
Aim: To evaluate the national patterns of use of AI-enabled prediction tools at US hospitals, and their association with hospital features and performance on cardiovascular outcome measures.
Methods: We leveraged the 2023 American Hospital Association (AHA) Annual IT Supplement. This included a national survey of US hospitals querying whether hospitals use EHR-integrated AI predictive models in care processes. We used AHA survey to identify a range of hospital characteristics, and linked the data to the CMS Hospital Quality Reports (2020–2023) to evaluate whether hospitals adopting these technologies represented those leading or lagging in cardiovascular performance measures, including risk-standardized 30-day mortality and readmission rates for acute myocardial infarction (AMI) and heart failure (HF). To assess these relationships, we used multivariable linear regression models adjusting for hospital characteristics.
Results: Among 2,885 hospitals in the AHA IT Survey, 1,085 (37.6%) reported using EHR-integrated AI-based predictive models, while 866 reported using only non-AI tools. The most common clinical applications of AI included predicting inpatient health trajectories (97.2%) and identifying high-risk outpatients for follow-up care (91.6%) (Figure 1). AI use was highest among hospitals with bedsize ≥300 (44.3% vs 37.2% in <100 beds), those located in the Northeast (42.5% vs 33.3% in the West), teaching (52.2% vs 36.2% non-teaching), and private hospitals (40.9% vs 23.1% government owned) (Figure 2). Hospitals with integrated AI technology, on average, reported a lower 30-day mortality rate for both AMI and HF, as well as modestly lower readmission rates for HF, but not AMI (Figure 3A). Hospitals reporting use of AI tools specifically for outpatient follow-up and treatment recommendation had lower readmission rates for both AMI and HF (Figure 3B).
Conclusions: Only a 3rd of US hospitals that participated in a national survey about health IT reported the use of EHR-integrated AI tools, with differential uptake across hospitals and use cases. There is a need for a national strategy to integrate and monitor health AI care systematically.
More abstracts on this topic:
A Novel Imaging Biomarker to Make Precise Outcome Predictions for Patients with Acute Ischemic Stroke
Mallavarapu Monica, Kim Hyun Woo, Iyyangar Ananya, Salazar-marioni Sergio, Yoo Albert, Giancardo Luca, Sheth Sunil, Jeevarajan Jerome
12-lead electrocardiograms predict adverse cardiovascular outcomes of emergency department patientsHaimovich Julian, Kolossvary Marton, Alam Ridwan, Padros I Valls Raimon, Lu Michael, Aguirre Aaron