Final ID: Su1093
Association of Patient Healthcare Information Exchange Systems at US Hospitals with 30-day Excess Days in Acute Care after Heart Failure Hospitalization
Abstract Body (Do not enter title and authors here): Background: Given its chronicity and high hospitalization burden, heart failure (HF) requires close coordinated care. Health Information Exchange (HIE) systems can improve care by enabling seamless information sharing between healthcare providers and patients. We evaluated whether hospitals that have invested in more comprehensive HIE access for patients have better risk-standardized post-discharge outcomes after HF hospitalization.
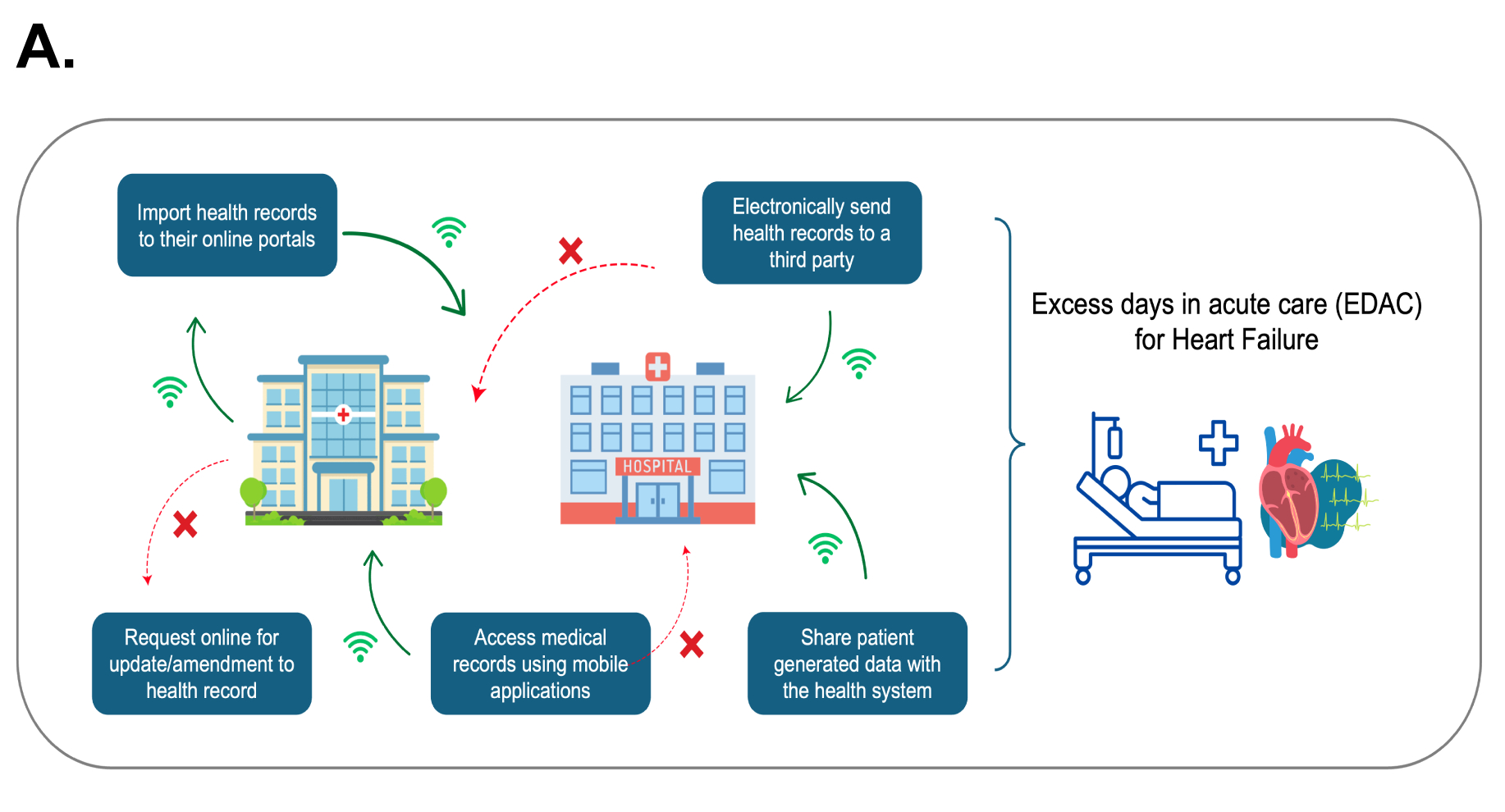
Methods: We defined a range of contemporary HIE services at all US acute care hospitals using the American Hospital Association (AHA) Information Technology (IT) Annual Survey (2022). HIE services included mobile access to health records, the ability to import, export, and update health records online, and the option to share patient-generated data with the health system, representing health measurements and data generated from smart devices (A). We identified each hospital’s corresponding 30-day excess days in acute care (EDAC) for HF – a risk-standardized metric of all acute care needs in the post-hospitalization period from the Centers for Medicare & Medicaid Services Quality Report (2019-2022) and examined the association between HIE services and 30-day EDAC for HF using multivariable linear regression.
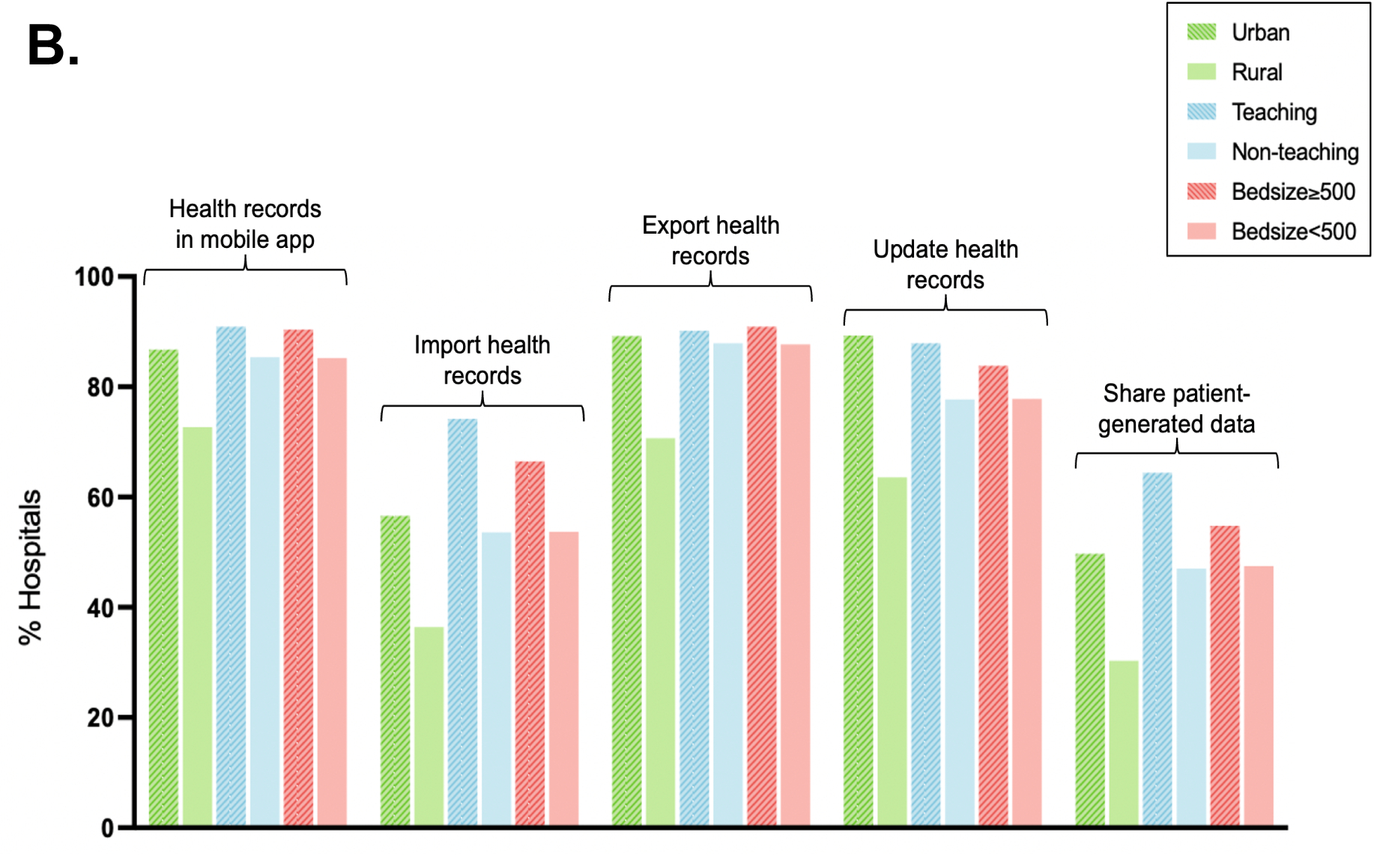
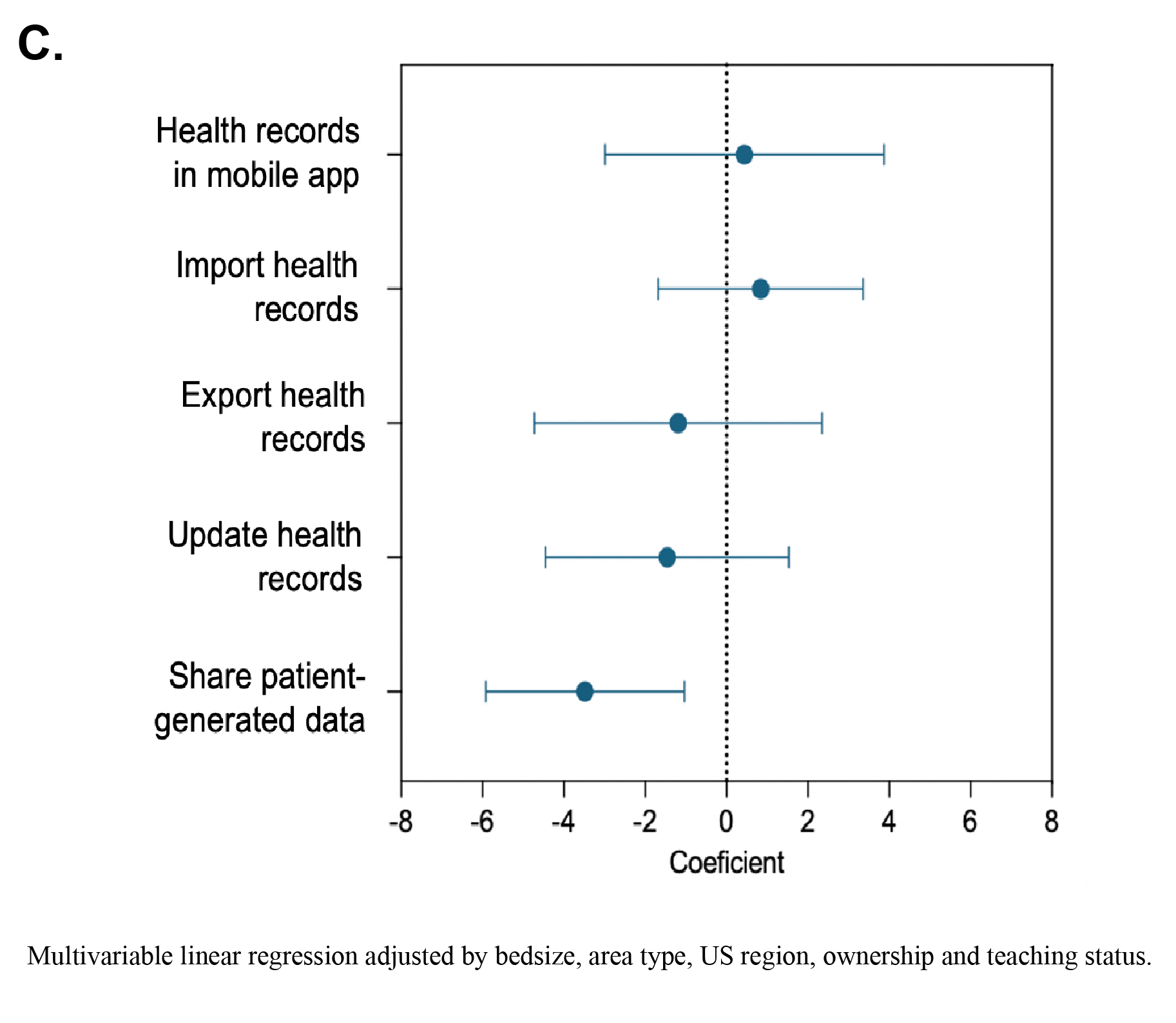
Results: There were 2,581 US hospitals (22% rural, 9% teaching, with a median bedsize of 162 [IQR 76, 307]) in the AHA-IT survey, with a median EDAC of 5.9 (IQR -8.6, 20.9) days for HF. The vast majority (99%) of hospitals had online health record portals, but access to specific HIE services varied widely across hospitals (B): 84% offered access via mobile application, 86% allowed data import, 55% data export to other health systems, and 77% online data updates, with fewer than half (47%) allowing patients to share patient-generated health data. After accounting for differences in hospital characteristics, only hospitals with HIE configured to enable patients to share their personal health data directly with the health system had significantly lower risk-standardized 30-day EDAC for HF (-3.9, 95% CI -1.04, -3.48) (C).
Conclusions: Hospitals with HIE services that include the sharing of patient-generated data have significantly better risk-standardized post-hospitalization outcomes for HF. There is a need to evaluate the role of broader access to bidirectional data sharing as a strategy to enhance care and outcomes at hospitals treating patients with ongoing post-discharge needs.
Methods: We defined a range of contemporary HIE services at all US acute care hospitals using the American Hospital Association (AHA) Information Technology (IT) Annual Survey (2022). HIE services included mobile access to health records, the ability to import, export, and update health records online, and the option to share patient-generated data with the health system, representing health measurements and data generated from smart devices (A). We identified each hospital’s corresponding 30-day excess days in acute care (EDAC) for HF – a risk-standardized metric of all acute care needs in the post-hospitalization period from the Centers for Medicare & Medicaid Services Quality Report (2019-2022) and examined the association between HIE services and 30-day EDAC for HF using multivariable linear regression.
Results: There were 2,581 US hospitals (22% rural, 9% teaching, with a median bedsize of 162 [IQR 76, 307]) in the AHA-IT survey, with a median EDAC of 5.9 (IQR -8.6, 20.9) days for HF. The vast majority (99%) of hospitals had online health record portals, but access to specific HIE services varied widely across hospitals (B): 84% offered access via mobile application, 86% allowed data import, 55% data export to other health systems, and 77% online data updates, with fewer than half (47%) allowing patients to share patient-generated health data. After accounting for differences in hospital characteristics, only hospitals with HIE configured to enable patients to share their personal health data directly with the health system had significantly lower risk-standardized 30-day EDAC for HF (-3.9, 95% CI -1.04, -3.48) (C).
Conclusions: Hospitals with HIE services that include the sharing of patient-generated data have significantly better risk-standardized post-hospitalization outcomes for HF. There is a need to evaluate the role of broader access to bidirectional data sharing as a strategy to enhance care and outcomes at hospitals treating patients with ongoing post-discharge needs.
More abstracts on this topic:
Association of Non-Cardiac Comorbidities With Long-Term Re-Hospitalization for Heart Failure: Contemporary Analysis of 88,528 Consecutive Cases
Ambrosio Giuseppe, Tagliabue Elena, Pellicori Pierpaolo, Lund Lars, Pontiroli Antonio
An Evaluation of Vascular Neurology Fellowship Websites: How Informed an Applicant Could Be?Sivakumar Milan, Degen Nathaniel, Varkey Thomas, Alexandrov Andrei, Singh Savdeep