Final ID: Sa2055
Insulin Sensitivity and Inflammation: Key Predictors of Cardiovascular Disease in Middle-Aged and Older Adults
Abstract Body (Do not enter title and authors here): Background: Cardiovascular disease (CVD) remains a leading cause of morbidity and mortality in middle-aged and older adults. Both the estimated glucose disposal rate (eGDR), and hs-CRP have been identified as important risk factors for CVD. However, their combined influence on CVD risk in this population remains inadequately explored.
Aim: This study aims to investigate the association between eGDR, hs-CRP, and the risk of CVD in middle-aged and older adults.
Methods:
Data were from the China Health and Retirement Longitudinal Study (CHARLS), which included 17,708 participants at baseline in 2011. After excluding those with cardiovascular disease (CVD) and missing follow-up data, 6,823 participants were enrolled. eGDR was calculated using the following formula: eGDR=24.31−(0.22×Waist Circumference)−(0.33×Systolic Blood Pressure)+(0.43×Fasting Plasma Glucose)eGDR=24.31−(0.22×Waist Circumference)−(0.33×Systolic Blood Pressure)+(0.43×Fasting Plasma Glucose). eGDR was categorized according to quartiles. The primary outcome was the incidence of heart diseases and stroke.
Results:
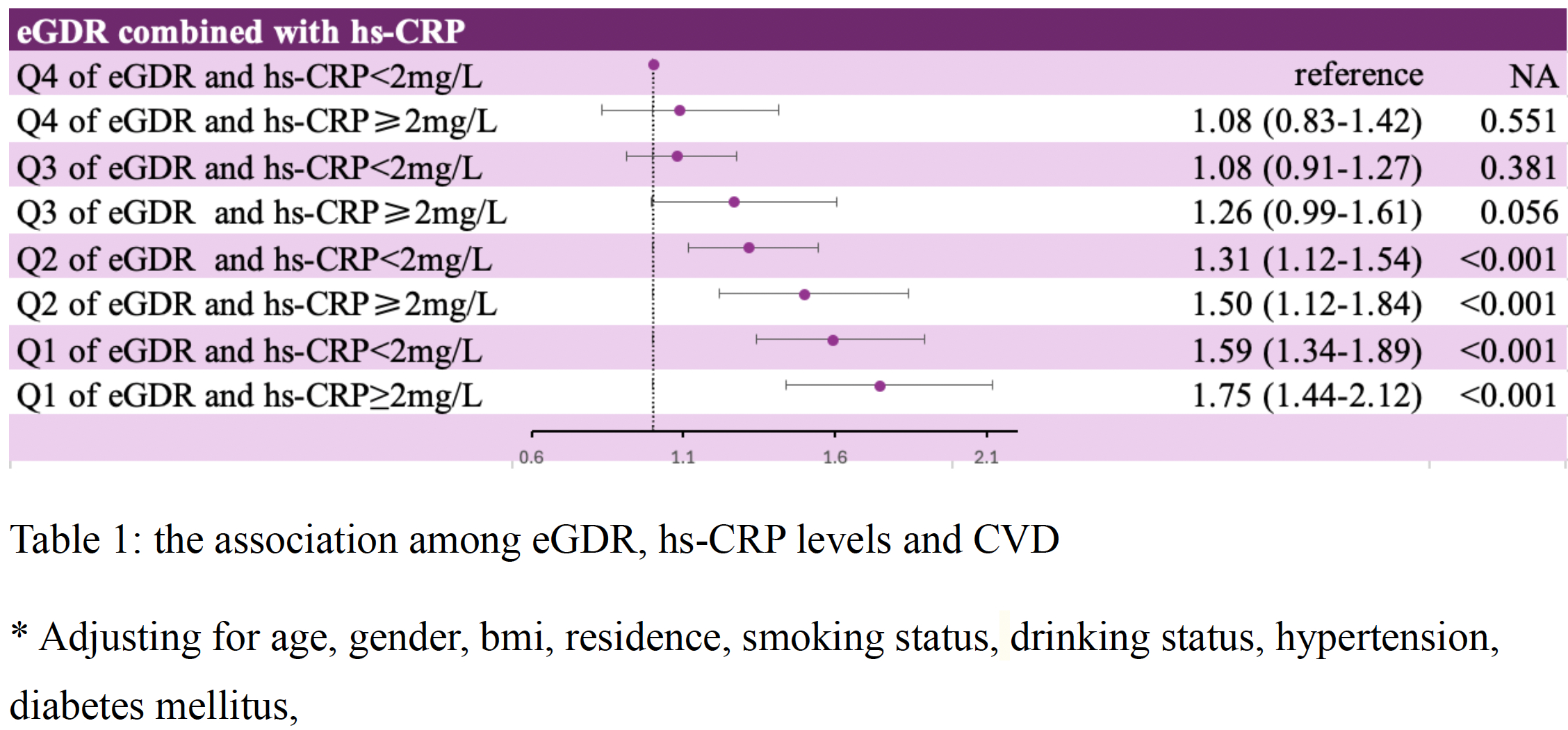
Among the 6,823 participants enrolled, the mean age was 59.14 ± 8.75 years, and 3,080 (45.1%) were male. During a maximum follow-up period of 9 years, 1,950 (28.6%) developed CVD. After adjusting for confounding factors, the risk of CVD incidence was highest in the lowest quartile (Q1) of eGDR compared to the highest quartile (Q4) (HR: 1.62, 95% CI: 1.38-1.88), followed by Q2 (HR: 1.34, 95% CI: 1.16-1.54). Elevated hs-CRP levels (≥2 mg/L) were associated with a 1.15-fold increased risk of CVD (95% CI: 1.04-1.27) compared to lower hs-CRP levels (<2 mg/L). When considering both eGDR and hs-CRP levels, the combined effect revealed the highest risk in individuals with the lowest eGDR (Q1) and elevated hs-CRP (HR: 1.75, 95% CI: 1.44-2.12), followed by those with Q1 of eGDR and low hs-CRP (HR: 1.59, 95% CI: 1.34-1.89), Q2 of eGDR with high hs-CRP (HR: 1.50, 95% CI: 1.22-1.84), and Q2 of eGDR with low hs-CRP (HR: 1.31, 95% CI: 1.12-1.54) (Table 1)
Conclusion:
In this large real-world study, we found that individuals with high eGDR and elevated hs-CRP had the highest risk of CVD. These findings highlight the combined role of insulin sensitivity and inflammation in predicting CVD risk and provide valuable insights into cardiovascular risk, aiding in early detection and targeted prevention strategies for CVD.
Aim: This study aims to investigate the association between eGDR, hs-CRP, and the risk of CVD in middle-aged and older adults.
Methods:
Data were from the China Health and Retirement Longitudinal Study (CHARLS), which included 17,708 participants at baseline in 2011. After excluding those with cardiovascular disease (CVD) and missing follow-up data, 6,823 participants were enrolled. eGDR was calculated using the following formula: eGDR=24.31−(0.22×Waist Circumference)−(0.33×Systolic Blood Pressure)+(0.43×Fasting Plasma Glucose)eGDR=24.31−(0.22×Waist Circumference)−(0.33×Systolic Blood Pressure)+(0.43×Fasting Plasma Glucose). eGDR was categorized according to quartiles. The primary outcome was the incidence of heart diseases and stroke.
Results:
Among the 6,823 participants enrolled, the mean age was 59.14 ± 8.75 years, and 3,080 (45.1%) were male. During a maximum follow-up period of 9 years, 1,950 (28.6%) developed CVD. After adjusting for confounding factors, the risk of CVD incidence was highest in the lowest quartile (Q1) of eGDR compared to the highest quartile (Q4) (HR: 1.62, 95% CI: 1.38-1.88), followed by Q2 (HR: 1.34, 95% CI: 1.16-1.54). Elevated hs-CRP levels (≥2 mg/L) were associated with a 1.15-fold increased risk of CVD (95% CI: 1.04-1.27) compared to lower hs-CRP levels (<2 mg/L). When considering both eGDR and hs-CRP levels, the combined effect revealed the highest risk in individuals with the lowest eGDR (Q1) and elevated hs-CRP (HR: 1.75, 95% CI: 1.44-2.12), followed by those with Q1 of eGDR and low hs-CRP (HR: 1.59, 95% CI: 1.34-1.89), Q2 of eGDR with high hs-CRP (HR: 1.50, 95% CI: 1.22-1.84), and Q2 of eGDR with low hs-CRP (HR: 1.31, 95% CI: 1.12-1.54) (Table 1)
Conclusion:
In this large real-world study, we found that individuals with high eGDR and elevated hs-CRP had the highest risk of CVD. These findings highlight the combined role of insulin sensitivity and inflammation in predicting CVD risk and provide valuable insights into cardiovascular risk, aiding in early detection and targeted prevention strategies for CVD.
More abstracts on this topic:
Blood Pressure Measures are Not Associated with Early Metabolic Imbalance: The U.S. National Health and Nutrition Examination Survey
Mendiola Luis, Dwivedi Alok, Cistola David
B-type Natriuretic Peptide Reverses Vascular Endothelial Insulin Resistance and Ameliorates Oxidative Stress in Human AtherosclerosisForan Daniel, Krasopoulos George, Srivastava Vivek, Sayeed Rana, Antonopoulos Alexios, Channon Keith, Akoumianakis Ioannis, Antoniades Charalambos, Badi Ileana, Polkinghorne Murray, Katsouda Antonia, Riering Marianne, Dalessio Andrea, Sastry Priya, Kourliouros Antonios, Walcot Nicholas