Final ID: MDP578
Impact of Neutrophil on Ischemic Risk in Acute Coronary Syndrome Patients Across Different Low Density Lipoprotein Cholesterol Levels
Abstract Body (Do not enter title and authors here): Background: Inflammation is a significant residual risk factor for coronary artery disease. While intensive lipid-lowering therapy has reduced the prevalence of plaque rupture, plaque erosion in acute coronary syndrome (ACS) patients is increasing, with neutrophils playing a crucial role. It remains unclear whether varying low-density lipoprotein cholesterol (LDL-C) levels modify the relationship between neutrophil count and ischemic risk in ACS patients.
Aim: To investigate the relationship between neutrophil counts and ischemic risk in ACS patients undergoing percutaneous coronary intervention (PCI) across different LDL-C levels.
Methods: This large cohort study enrolled consecutive 10724 patients undergoing PCI at Fuwai Hospital (Peking Union Medical College) throughout the year of 2013. Patients were divided into subgroups according to baseline LDL-C levels, with cut-off points at 1.8mmol/L or 1.4mmol/L. The primary endpoint was major adverse cardiovascular event (MACE), and the secondary endpoint was revascularization.
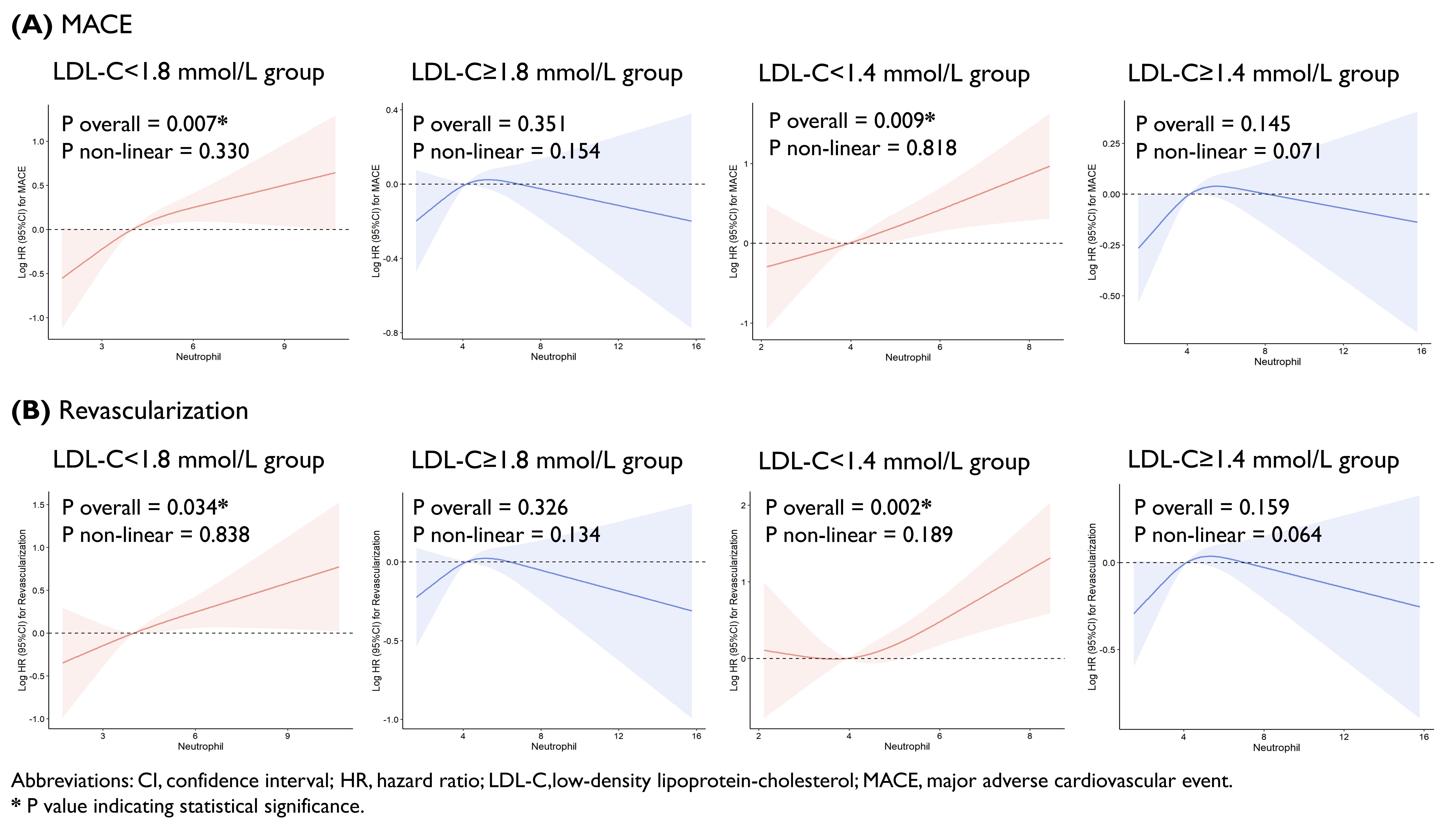
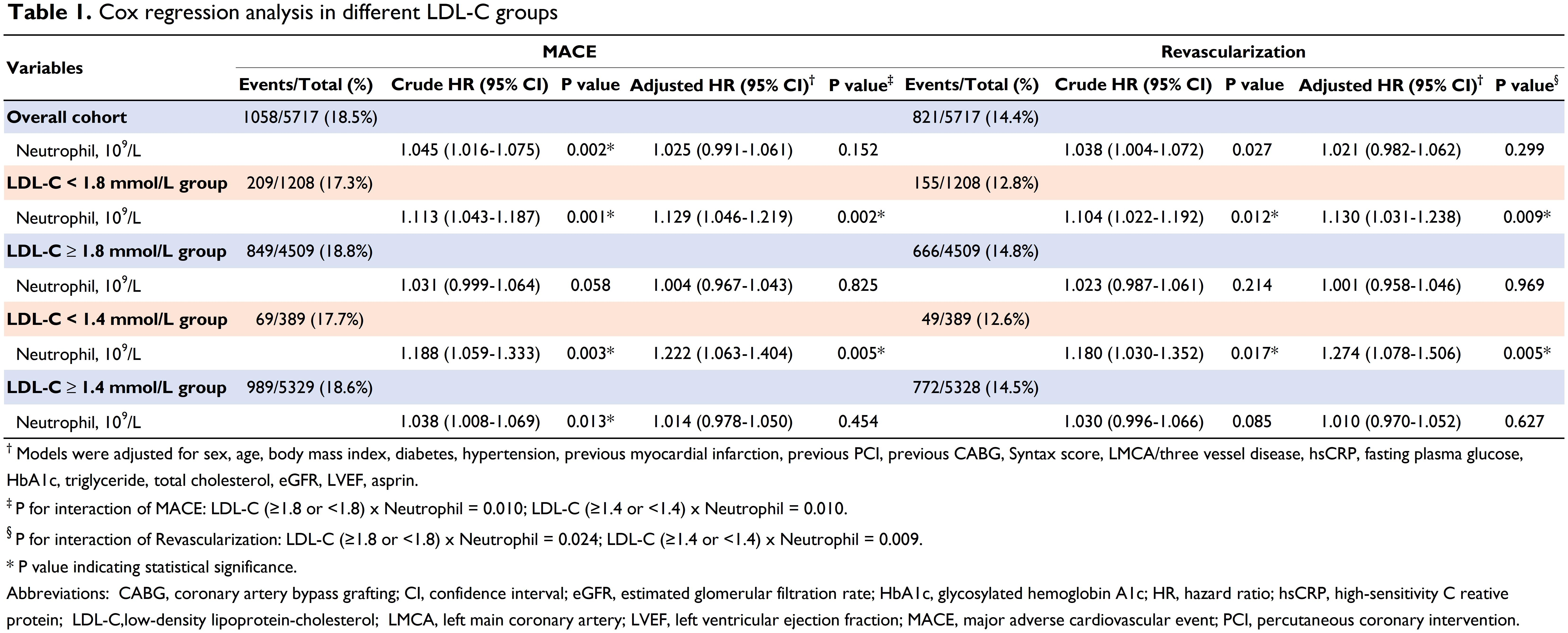
Results: Finally, 5717 ACS patients with PCI were included. The mean age was 58.43 ± 10.35 years, with 4399 (76.9%) being male. During the 5-year follow-up period, 1058 (18.5%) MACEs and 821 (14.4%) revascularizations were recorded. Restricted cubic spline analysis revealed a positive correlation between neutrophil and MACE and revascularizations only in patients with lower LDL-C levels (LDL-C <1.8 and LDL-C <1.4 mmol/L), but not in those with higher LDL-C levels (LDL-C ≥1.8 and LDL-C ≥1.4 mmol/L) (Figure 1). Multivariate Cox regression analysis showed that in the LDL-C <1.8 mmol/L group, each unit increase in neutrophil count was associated with a 1.129 times higher risk of MACE (HR 1.129; 95% CI 1.046-1.219) and a 1.130 times higher risk of revascularizations (HR 1.130; 95% CI 1.031-1.238). Similar findings were observed in the LDL-C <1.4 mmol/L group, where higher neutrophil was independent risk factors for MACE (HR 1.222; 95% CI 1.063-1.404) and revascularizations (HR 1.274; 95% CI 1.078-1.506). However, in patients with higher LDL-C levels (LDL-C ≥1.8 and LDL-C ≥1.4 mmol/L), neutrophil counts were not associated with outcomes (Table 1).
Conclusions:High neutrophil counts are a significant risk factor for ischemic events in ACS patients with low LDL-C levels, highlighting the potential benefits of targeting neutrophils-related inflammatory pathway in the management of ACS patients with well-controlled LDL-C levels.
Aim: To investigate the relationship between neutrophil counts and ischemic risk in ACS patients undergoing percutaneous coronary intervention (PCI) across different LDL-C levels.
Methods: This large cohort study enrolled consecutive 10724 patients undergoing PCI at Fuwai Hospital (Peking Union Medical College) throughout the year of 2013. Patients were divided into subgroups according to baseline LDL-C levels, with cut-off points at 1.8mmol/L or 1.4mmol/L. The primary endpoint was major adverse cardiovascular event (MACE), and the secondary endpoint was revascularization.
Results: Finally, 5717 ACS patients with PCI were included. The mean age was 58.43 ± 10.35 years, with 4399 (76.9%) being male. During the 5-year follow-up period, 1058 (18.5%) MACEs and 821 (14.4%) revascularizations were recorded. Restricted cubic spline analysis revealed a positive correlation between neutrophil and MACE and revascularizations only in patients with lower LDL-C levels (LDL-C <1.8 and LDL-C <1.4 mmol/L), but not in those with higher LDL-C levels (LDL-C ≥1.8 and LDL-C ≥1.4 mmol/L) (Figure 1). Multivariate Cox regression analysis showed that in the LDL-C <1.8 mmol/L group, each unit increase in neutrophil count was associated with a 1.129 times higher risk of MACE (HR 1.129; 95% CI 1.046-1.219) and a 1.130 times higher risk of revascularizations (HR 1.130; 95% CI 1.031-1.238). Similar findings were observed in the LDL-C <1.4 mmol/L group, where higher neutrophil was independent risk factors for MACE (HR 1.222; 95% CI 1.063-1.404) and revascularizations (HR 1.274; 95% CI 1.078-1.506). However, in patients with higher LDL-C levels (LDL-C ≥1.8 and LDL-C ≥1.4 mmol/L), neutrophil counts were not associated with outcomes (Table 1).
Conclusions:High neutrophil counts are a significant risk factor for ischemic events in ACS patients with low LDL-C levels, highlighting the potential benefits of targeting neutrophils-related inflammatory pathway in the management of ACS patients with well-controlled LDL-C levels.
More abstracts on this topic:
A drug target Mendelian randomization study of triglyceride lowering therapies for aortic stenosis
Ciofani Jonathan, Han Daniel, Gill Dipender, Rao Karan, Allahwala Usaid, Bhindi Ravinay
A Mast Cell-Specific Receptor Mediates Post-Stroke Brain Inflammation Via a Dural-Brain AxisKothari Ruchita, Caplan Justin, Gonzalez L. Fernando, Jackson Christopher, Bettegowda Chetan, Huang Judy, Koehler Raymond, Tamargo Rafael, Xu Risheng, Dong Xinzhong, Abdulrahim Mostafa, Oh Hyun Jong, Capuzzi Daniel, Nair Sumil, Zhang Yaowu, Limjunyawong Nathachit, Saini Sarbjit, Kim Jennifer